News
COVID-19 update clinics:
The BSS team ensures that our treatment rooms and equipment are wiped and sanitized after each patient. We follow the government guidelines and we are keen to reassure you that in addition to the very high standards and regulations already in place , we are taking additional steps to ensure your visit to the clinic is safe.
- We work on a strict appoint-only basis in order to minimize crowding in the clinic.
- You must wear a mask prior to arrival ( mask can be bought at the chemistry on the ground floor for 2€)
- Please visit the clinic alone ( kids and companions will refused access to the clinic)
The BSS team is following stringent hand hygiene policies using gloves ,masks and face shields if needed. Hand sanitizers are also available at the reception and in every room. Although these are unfamiliar times to everyone, we will always remain committed to prioritizing the health and safety of both patients and staff.
UK clinics will be open once government restrictions have been listed.
We look forward to seeing you soon.
The BSS Team

World Obesity Federation
More than half the world's population will be classed as obese or overweight by 2035 if action is not taken, the World Obesity Federation warns.
More than four billion people will be affected, with rates rising fastest among children, its report says.
Low or middle-income countries in Africa and Asia are expected to see the greatest rises.
The report predicts the cost of obesity will amount to more than $4tn (£3.3tn) annually by 2035.
The president of the federation, Prof Louise Baur, described the report's findings as a clear warning to countries to act now or risk repercussions in the future.
The report in particular highlights the rising rates of obesity among children and teenagers, with rates expected to double from 2020 levels among both boys and girls.
Prof Baur said the trend was "particularly worrying", adding that "governments and policymakers around the world need to do all they can to avoid passing health, social, and economic costs on to the younger generation" by assessing "the systems and root factors" that contribute to obesity.
The effects of obesity's prevalence on lower-income countries is also highlighted in the report. Nine of the 10 countries with the greatest expected increases in obesity globally are low or lower-middle income states in Africa and Asia.
Reasons include trends in dietary preferences towards more highly processed foods, greater levels of sedentary behaviour, weaker policies to control food supply and marketing, and less well-resourced healthcare services to assist in weight management and health education.
Lower-income countries are "often the least able to respond to obesity and its consequences".
The findings estimate that rises in obesity rates around the world will have a significant impact on the global economy, equating to 3% of global Gross Domestic Product.
The report emphasises that its acknowledgement of the economic impact of obesity "is in no way a reflection of blame on people living with obesity".
The data published in the report will be presented to the UN on Monday.
Obese is a medical term used to describe a person with a high excess of body fat.
Read more

Bariatric Surgery vs. weight management
Surgery remains the most effective and cost-effective long-term approach to reducing weight for adults adults with severe obesity, according to research from the University of Aberdeen, Aberdeen, UK Health Forum, London and the University of Oxford, Oxford, UK. However, the study also found that high quality weight management programmes (WMPs) are effective tools in reducing weight for up to 10 years in some cases.
"The purpose of this study was to examine the available evidence looking at the effectiveness and cost-effectiveness of different weight management procedures from the perspective of the NHS,” said lead author, Professor Alison Avenell from the University of Aberdeen. "Whilst the study shows that surgical interventions remain much more effective, provision of surgery for obesity management by the NHS is presently very low. Other weight management programmes can be effective in terms of helping people who are severely obese lose weight and are cost-effective for the NHS."
The outcomes of the REBALANCE study, were published in the paper, ‘Bariatric surgery, lifestyle interventions and orlistat for severe obesity: the REBALANCE mixed-methods systematic review and economic evaluation’, which was funded by the National Institute for Health Research (NIHR). In the study, the researchers reviewed 236 studies looking at evidence for acceptability, effectiveness and value for money of surgery, diet and exercise weight management programmes, and the drug orlistat.
They undertook four systematic reviews, which were of:
- Randomised controlled trials (RCTs) or quasi-randomised trials of bariatric surgery, lifestyle WMPs and orlistat (approved by the National Institute for Health and Care Excellence) with mean or median follow-up durations of ≥ 12 months. We included comparisons between interventions or comparisons with usual care/controls.
- UK lifestyle WMPs and orlistat with any study design and a mean or median follow-up duration of ≥ 12 months.
- Qualitative and mixed-methods research on the feasibility and acceptability of lifestyle WMPs and orlistat (including views of professionals involved in care).
- Economic evaluations (trial analyses and decision modelling studies) of bariatric surgery, lifestyle WMPs and orlistat.
- Data from the systematic review of RCTs populated a microsimulation model predicting costs, outcomes and cost-effectiveness of the most-effective programmes over a 30-year time horizon from a NHS perspective for a population representative of all adults with a BMI of ≥ 35 kg/m2. The UK Health Forum microsimulation model assessed the cost-effectiveness of:
- the Look AHEAD trial WMP versus baseline UK general population BMI trends
- a very low-calorie diet (VLCD) added to a WMP versus a WMP alone, with both versus the baseline UK general population BMI trend
- Roux-en-Y gastric bypass (RYGB) versus a WMP, with both versus the baseline UK general population BMI trends.
The outcomes were weight change (primary outcome), cardiovascular risk factors, psychological well-being, adverse events, quality of life, process outcomes, qualitative outcomes, costs and economic evaluations.
Outcomes
The reported that bariatric surgery, especially RYGB, produced greater long-term weight change than any of the WMPs [RYGB mean –20.23kg, 95% confidence interval (CI) –23.75 to –16.71kg] at 60 months. Adding a VLCD to an existing WMP gave an additional mean weight change of –4.41kg (95% CI –5.93 to –2.88 kg) at 12 months. Orlistat and dietary counselling reduced weight regain after VLCDs. Long-term weight maintenance after weight-loss programmes that did not incorporate VLCDs was improved by orlistat and follow-up in person or by telephone.
Data analyses initially favoured low-carbohydrate (< 40 g/day) reducing diets compared with low-fat reducing diets (mean weight change of –1.16 kg, 95% CI –2.13 to –0.19kg), and higher protein (≥ 30% energy) reducing diets compared with lower protein reducing diets (mean weight change of –0.91 kg, 95% CI –1.83 to 0.00kg) at 12 months, but not beyond 12 months. The use of meal replacements, such as giving component parts of VLCDs, was associated with greater weight loss, but only at 12 months (mean weight change of –2.75kg, 95% CI –4.01 to –1.48kg).
More intensive interventions, with more contacts with WMP personnel (in person or remotely), were usually associated with greater weight loss and better weight maintenance. Initial inpatient programmes were not associated with greater weight loss. Interventions delivered to groups rather than to individuals had greater weight loss results, but groups usually had more contacts. There was little evidence that incorporating family members for support and modifying the home environment were beneficial. Similarly, interventions that were weight neutral or did not target weight loss were less effective than those with a prescribed calorie content or deficit.
In summary, they reported that:
- Bariatric surgery had the best long-term weight-loss results and could be a good use of NHS resources, compared with no surgery or weight management programmes on their own.
- Of non-surgical approaches, very low-calorie diets produced the best weight-loss result at 12 months, but it was unclear if weight-loss was any greater than standard WMPs for longer than this.
- Adding a very low-calorie diet to an existing weight management programme was shown to not be a good use of NHS resources. However, most weight management programmes, including those with very low-calorie diets, appeared to be a good use of NHS resources compared with doing nothing at all.
- Low-carbohydrate Atkins-type diets, higher protein intakes or the use of meal replacements had small added effects on improving weight loss compared to other WMPs at 12 months. They also found no evidence that they were better than other diets after 12 months.
- The best result for long-term non-surgical weight loss (over nearly 10 years) came from an intensive WMP with all of the following: a low-fat reducing diet, a calorie goal of 1200–1800 kcal/day, initial meal replacements or meal plans, a tailored exercise programme, cognitive behavioural therapy, intensive group and individual support, and follow-up by telephone or e-mail. However, this type of WMP would be more costly for the NHS than simpler WMPs.
- Other components of effective interventions included increasing physical activity to help prevent long-term weight regain and receiving longer-term help with diets or using the drug orlistat. Adding telephone or internet support, and group support, also helped to keep weight off.
- Participants in weight management programmes valued novelty, weight management programmes endorsed by health-care providers and belonging to a group of people who shared similar issues.
In addition, they noted that weight-management programmes were generally cost-effective compared with a baseline of current UK general population obesity trends [incremental cost-effectiveness ratio < £20,000/quality-adjusted life-year (QALY)]. However, the addition of a VLCD to a WMP was not cost-effective. The Look AHEAD programme was borderline cost-effective compared with current population obesity trends, with an improved case for cost-effectiveness under longer-term weight regain assumptions.
RYGB was the most cost-effective strategy overall in the base-case analysis, over a 30-year time horizon, although the model did not replicate long-term cost savings for surgery suggested by some studies in systematic review. The economic model results were sensitive to assumptions about weight regain, model time horizon and discount rates for costs and QALYs.
Read more

Increasing access to surgery and preventing post-op weight regain
Owen Haskins - Editor in chief, Bariatric News
In a wide-ranging interview, Bariatric News talked to Mr Shaw Somers, upper gastrointestinal and bariatric (metabolic) Consultant Surgeon with Streamline Surgical and President of the British Obesity & Metabolic Surgery Society (BOMSS), about the lack of access to surgery, the need to educate people on the causes of obesity and how to treat post-operative weight regain.
shaw_somer2.png

Shaw Somers
“The problem we face in the UK is of a publicly-funded health system in which the government absolutely dictate what and who we can and can’t operate on, based on money,” Mr Somers began. “Unfortunately, we still have a disconnect in the UK between what the National Institute for Health and Care Excellence (NICE) guidance states and what politicians and the people within NHS England are prepared to accept as standards of care. We have NICE guidance which is very clear on how and what we should be spending money on in terms of treating obesity and yet it seems to be completely voluntary for commissioners to opt out of if they want. We now have less Tier 4 commissioned surgery than we did three years ago and only 44% of all commissioning groups procure bariatric services.”
He believes the lack of awareness about the causes of obesity and how to treat obesity comes down to a lack of education, as many people do not understand that obesity is a disease, and stated that it is up to obesity specialists including bariatric surgeons, researchers, nurses, dieticians etc to educate colleagues, politicians, policy-makers, commissioning groups, the media and the public that obesity is an illness - rather than a lifestyle choice.
Obesity is not a lifestyle choice
“I have met thousands of people with obesity and not one of them choose to be obese. Our great challenge will be to convince people that obesity is a disease and that there are treatments available that work,” said Mr Somers. “To ask people to eat less and exercise more is a ridiculous over simplification of the scientific evidence and is ignoring the fact that much of your weight is determined by genetics. I think we need to start exposing fat shaming for what it is - and that is the prejudice of ignorance - it does not work to help people lose weight, in fact it is counterproductive.”
He emphasised that BOMSS is still very busy behind the scenes lobbying the various stake-holders to raise awareness and try and improve access to all treatments for obesity, and will continue to work hard on behalf of the bariatric community to educate and demonstrate that bariatric procedures are safe, effective and have not only resulted in reducing the weight of tens of thousands of people over the years but have also improved their overall health and quality of life by reducing their co-morbidities, and improving quality of life.
"There is also evidence that shows sleeve and bypass procedure tend to fade with time, this ‘fatigue’ or loss of restriction means the restrictive and hormonal effects of the procedure diminish over time.”
He explained that people need to understand the nature of obesity as an illness and that obesity is about how our brain perceives food and satisfaction, and when that relationship becomes disordered, we start to eat more. Mr Somers added that is not because we are inherently greedy but because our brain does not respond in the way it should to food. The reason for this are multifactorial including the type of food we eat, the stresses of modern day life, mental illness - including anxiety and depression – all change the way the brain functions, and this includes the way the brain responds to food.
Bariatric and metabolic surgery
He explained that there is growing evidence that there is not one mechanism for bariatric surgery’s effects but many. He said that surgery’s effects are not just hormonal, not just restrictive and not just a change is the patient’s dietary habits and lifestyle – it is a combination of all three. He believes that there are three phrases to bariatric surgery’s effects:
1) There is an initial ‘shock and awe’ phase that changes a patient’s experience when the eat after the procedure, which includes a feeling of restriction.
2) A phase of hormonal effects where the actual physiology of the bariatric procedure changes how the patient feels and how they work with food, and;
3) The longer-term dietary rehabilitation and the longer-term effects of surgery that either help the patients maintain their habits or not - and it is here where weight regain occurs.
There are now many tens of thousands of people in the UK that have had successful bariatric procedures, unfortunately the human body adapts and changes over time, and these changes bring with it the possibility of weight regain.
According to Mr Somers, the first two phases work because of the restrictive effects of the procedure, depending on the procedure. If either the physical or hormonal effects are no longer present, this is when weight regain occurs. The question then becomes: How do you maintain the effects of the operation in the long-term? One solution is to maintain restriction.
“We know from long-term gastric band data that if the band is still in place and there have not been any complications then the outcomes are good, and there are several long-term gastric band studies that are at least as good as the long-term sleeve and bypass data. We know that once band patients are stable they don’t regain weight because the band is still working and is having an effect. There is also evidence that shows sleeve and bypass procedure tend to fade with time, this ‘fatigue’ or loss of restriction means the restrictive and hormonal effects of the procedure diminish over time.”
The ‘banded procedure’
One possible way to prevent ‘surgical fatigue’ and maintain restriction is to perform a ‘banded bypass’ or ‘banded sleeve’, in which a surgeon places a band or a MiniMizer Ring (Bariatric Solutions) around the gastric pouch to prevent pouch dilatation.
According to Mr Somers, patients who have a MiniMizer Ring find that the ‘fatigue’ effect does not occur as they still have an element of restriction and that stops weight regain in the long-term. Whilst the initial phases weight loss for ‘banded’ patients is generally the same as non-banded patients, it is the prevention of long-term weight regain that is the real benefit of using a device such as the MiniMizer Ring.
Mr Somers has been using the MiniMizer Ring for about three years and has performed about 40 - all private cases - as the MiniMizer Ring is not freely available on the NHS.
“I routinely offer the MiniMizer Ring to patients if they are undergoing a revision procedure from a band to a bypass, as the one thing they complain about is a loss of restriction and they don’t feel comfortable working with no restriction element,” he explained. “I believe that is one of the indications for a Ring – patients who have had a previous gastric band. I would also recommend a banded bypass in primary bypasses cases in superobese patients, as the procedure offers a much more durable restriction effect. When the bypass naturally fatigues - because all tissues soften and stretch with time – the added restriction of the MiniMizer Ring ‘protects’ the bypass and reduces the feeling that the restrictive effect has faded.”
He said that he particularly likes the MiniMizer Ring compared to a band as the Ring is easy to apply and calibrate, adding that he has had no complications using the MiniMizer Ring with regards to slippage or erosions, however using an inflatable band for a banded bypass he has had some complications.
“I think the adjustability aspect of bands means than you can over adjust the band and that is when patients will start to struggle this can lead to slippage, migration or dilatation of the pouch above the band which goes against the very reason you placed the band in the first place. The MiniMizer is easy to apply and is placed and fixed so it is ‘snug’ next to the pouch - but not tight - leaving enough space to allow the food to pass through. That is the beauty of the procedure – it is very simple and it seems to works!”
Feedback from patients who have received a Ring after revision surgery reveals that they are happy, because they have a restriction that they can work with. Patients without the Ring are not as happy as they notice the restriction waning as the procedure starts to fatigue.
Managing expectations
Mr Somers explained that another important aspect to surgery is managing patient’s expectations but also difficult because as a surgeon one does not want to put them off the procedure by mentioning weight regain otherwise they will think, ‘Well what’s the point?’
He said that ‘managing expectation’ is a discussion all surgeons should have with their patients, but it should be handled in an honest way and one should approach the conversation from the view that weight regain is a ‘probability’ rather than a ‘possibility’ in the longer term. He said that in discussions with patients, surgeons should be explicit that they are offering patients a tool that can provide a remission from their obesity, rather than a cure.
“I use the analogy of patients being given a new musical instrument. They will need to learn about it and be trained to use it if they are going to get any kind of music,” he concluded. “Furthermore, as the years go by they may need to renew their instrument, or even upgrade. The principle is the same for bariatric surgery.”
Read more
Living with bariatric surgery
In April 2017, Dr Denise Ratcliffe, a Consultant Clinical Psychologist at Phoenix Health, UK and previously at Chelsea & Westminster Hospital, London, UK released her new self-help book: ‘Living with Bariatric Surgery - Managing your mind and your weight’, to help those who are considering bariatric surgery develop the psychological tools to make the necessary changes and adjustments for surgery to be successful. Bariatric News talked to Dr Ratcliffe about the aims of her book, the importance of understanding eating patterns and how managing post-surgical expectations can help people cope with the life changing aspects of bariatric surgery.
“Unfortunately, most people do not have regular or ongoing access to a psychologist when they are going through a bariatric surgery programme, so the aim of the book is to try and address that gap. I have worked in this area for over ten years and the book is really a culmination of all my knowledge and experience in the field,” Dr Ratcliffe began. “The target audience are patients who are in the process of having surgery as well as being a resource for those who have undergone surgery to help them adapt to the physical, psychological and relationship adjustments that occur. It will also be useful for health professionals who are new to the area and who want to find out more about the psychological aspects of bariatric surgery.”
denise_radcliffe_ol.jpg

Denise Ratcliffe
Although the benefits of bariatric surgery are significant, the psychological challenges it can present for patients have been overlooked. Consisting of 12 chapters in over 200+ pages, the book helps patients develop a realistic view of bariatric surgery and the changes required so they can adapt to life after surgery.
“There are no exact numbers on how many patients have access to a psychologist, but for most patients they will have a pre-operative assessment and perhaps some limited post-operative consultation. This lack of post-operative psychological input is very important as it is post-operatively where most of the psychological issues tend to arise.”
"We ask patients to look at what they want from surgery – more often than not weight loss is a proxy for something else – it is more important to them that they feel healthy, be more active with their children, be able to move more freely. Weight is just a number at the end of the day – whereas playing with their children is the real reward.”
According to Dr Ratcliffe, it is important that patients make the necessary psychological changes before and after surgery so that they are better prepared to negotiate the adjustments and achieve their goals, as well as helps normalise some of the issues that they might experience.
Bariatric myths
She explained that there are several myths surrounding bariatric surgery - one of the most common is that surgery will prevent patients from eating and they will never be able to put weight on again. A second myth is that after losing weight, patients will finally be happy and that all their problems will disappear.
“There is also a perception that bariatric surgery is somehow the ‘easy option’ – so some patients feel guilty or ashamed because they feel they are taking the easy route by having surgery – when actually they are choosing the most evidence-based treatment available.”
Many bariatric patients present with a range of psychological conditions ranging from binge-eating and emotional eating patterns, to depression and weight-related anxiety. Psychological difficulties that have occurred as a consequence of weight stigma are particularly prevalent. These psychological difficulties are often longstanding, with some going back to childhood experiences of abuse and/or neglect. These issues can impact on the type of coping mechanisms that people develop.
“By the time the psychologist gets to meet them, people are often very focused on getting the operation. Quite often they have tunnel vision – they think about the surgery and losing weight and its hard to see beyond that,” she added. “They often cannot imagine what the consequences may be in terms of body image, changing their relationship with food, possible impact on their relationships with friends and family etc. It really is a journey of self-discovery – and there are lots of issues that can arise from surgery. On balance, most people get a real benefit from surgery, but patients need to understand that it is inevitable that there are going to be challenges and set-backs along the way.”
Dr Ratcliffe said it is often difficult for patients to imagine the issues and challenges that may arise after surgery, as they have often had to fight very hard to access the surgery or they have been very focused on losing weight because that is the problem they are trying to address. Therefore, it is essential patients are made aware of what the consequences of surgery might be and that they research possible consequences, as well as speak to other patients who have had surgery.
“For most patients, when they visit a psychologist it is the first time they have had an opportunity to think about the psychological aspects of their eating behaviour. Usually, they have done every diet under the sun and they have really good knowledge about what is in food, what they should and should not eat. However, it is their psychological relationship with food – whether it is emotional eating patterns or binge eating etc – that they often need to address. Many patients use food as a mechanism to cope, so their relationship with food needs to be addressed.”
Moreover, she stressed that it is important that patients think about actively managing mood issues, such as depression and anxiety, either before or alongside surgery. These are not necessarily factors which should prevent people from having surgery, she added, but it is vital that patients are aware so they are able to anticipate, recognise and manage themselves after surgery. By identifying these issues and how they are linking to eating, healthcare professionals can then help patients develop strategies and coping mechanisms, so patients can manage their issues in a different way rather than defaulting to their usual patterns.
Managing expectations
She explained that surgery is about appreciating both the positive aspects and the challenging aspects, so patients comprehend that surgery and the subsequent weight loss is not going to solve all of their problems and make them appreciate that patients will encounter some unexpected challenges and problems along the way.
“Managing expectations around weight loss is fundamental, many patients think that they will get into BMI <25 range. If they do not achieve that they often think that they have failed. So, it is important to communicate what is realistic and what is likely, it is a balance of positive aspects and challenging aspects. We ask patients to look at what they want from surgery – more often than not weight loss is a proxy for something else – it is more important to them that they feel healthy, be more active with their children, be able to move more freely. Weight is just a number at the end of the day – whereas playing with their children is the real reward.”
Dr Ratcliffe explained that many patients do not ‘update’ their body image after surgery, so they look in the mirror and see themselves as the same size that they were before surgery. It can take the brain some time to catch up and she encourages patients to gather accurate information such as taking photos, paying attention to their new clothes size and noticing things they are physically able to do that were previously not possible.
“Many patients are also incredibly self-critical about their appearance before surgery and this can continue post-operatively, so we try to get patients to step back from this mindset and focus on the positive aspects such as noticing what the body can do now, the improvements in how the body functions and what patients can do physically after surgery – such as walking up the stairs without becoming breathless - compared to before surgery.”
Excess skin is a really serious problem for many people post-operatively and can be extremely distressing, making people feel even more distressed about their body and their appearance after surgery. It is extremely difficult to access funding for body contouring surgery and so Dr Ratcliffe helps patients to find ways of coping with this (whilst also being realistic about how challenging this is).
“By working on the changes before surgery, patients undergo a much smoother transition. It is like training for a marathon, you would never just get up and run 26 miles, you have to do the training and preparation before-hand, it is really about synching a patients’ behaviour with the post-operative requirements.”
“In some cases, it is those patients who have been the most adherent to their post-surgical programme that present with excess skin. We all have positive, neutral and negative aspects and thoughts about our body and appearance. Many people have got used to being highly self-critical about their image so we ask them to step back and also pay attention to the neutral and positive aspects that they may be overlooking.”
Relationships
Bariatric surgery can have a considerable impact on relationships - in positive and negative ways and this is something patients need to be prepared for. Some of the changes can be unexpected – sometimes there can be elements of jealousy from friends and partners, especially if they struggle with their weight as well. For example, they may encourage them to eat inappropriate foods, so people need to think ahead, be aware this may happen and have a plan of what to do in that situation.
“This is particularly evident in relationships where people are overweight and as one starts to lose weight after surgery, this can cause tension as one partner tends to feel left behind as their partner moves on and more things become possible,” she added. “If there were problems in the relationship before this can become more of an issue post-operatively. It does not tend to impact people who are in happy and functional relationships before surgery.
In addition, she highlighted that often people avoid certain situations because of their weight, so after surgery they encounter new situations and relationships, and often they need support in how to form new relationships, as well as develop their confidence in new social situations, and quite often this will mean learning new skills.
“The process is all about making healthy changes and developing new habits. Bariatric surgery is only a tool and we know that the effects of the surgery will wane over time. Therefore, it is the behavioural aspects that are fundamental to achieving long-term success, patients who implement and adhere to those behavioural changes have much better outcomes, than those patients who are non-adherent,” she concluded. “By working on the changes before surgery, patients undergo a much smoother transition. It is like training for a marathon, you would never just get up and run 26 miles, you have to do the training and preparation before-hand, it is really about synching a patients’ behaviour with the post-operative requirements.”
To order your copy of ‘Living with Bariatric Surgery: Managing your mind and your weight’ by Dr Denise Ratcliffe, please visit the publisher here or purchase from Amazon here
Read more

Bariatric surgery could have an impact on relationship status
Two new Swedish studies have reported that bariatric surgery could have an impact on relationships, with one finding that major weight loss after bariatric surgery was associated with more divorces, and a second study noting that singles were more likely to form new relationships or marry after a weight-loss operation.
"Those of us who take care of bariatric surgery patients notice that many patients experience a pretty profound change in their lives," said Dr Luke Funk, an assistant professor of surgery at the University of Wisconsin in Madison, and co-author of an editorial published with the study. "Their significant weight loss and improvements in other health problems, like high blood pressure and diabetes, cause changes in both their physical and mental well-being. They often take up new hobbies, become much more physically active, and feel much more confident about themselves. They also tend to have an improved self-image. I think this leads many to re-examine their relationships with others.”
One of the new studies, tracked the relationship histories of nearly 2,000 obese Swedish patients who underwent bariatric surgery over ten years. The investigators compared patients from the Swedish Obese Subjects (SOS) study with about 1,900 obese adults who did not have surgery. The other study using data from the Scandinavian Obesity Surgery Registry (SOReg) - looked at post-surgical data on about 29,000 patients who underwent gastric bypass surgery and compared with over 280,000 individuals in the general public, three years post-surgery.
The study authors found that bariatric surgery was tied to increased odds for divorce or separation for those in a prior relationship, especially for those who lost the most weight. Among those who had been unattached, significant weight loss was associated with higher odds for a new relationship or marriage. The report, ‘Associations of Bariatric Surgery With Changes in Interpersonal Relationship Status: Results From 2 Swedish Cohort Studies’, published in JAMA Surgery.
The SOS study included 1,958 patients who had bariatric surgery (of whom 1,389 [70.9%] were female) and 1,912 matched obese controls (of whom 1,354 [70.8%] were female. The SOReg cohort included 29,234 patients who had gastric bypass surgery (of whom 22,131 [75.6%] were female) and 283,748 comparators from the general population (of whom 214,342 [75.5%] were female).
"Unfortunately, our study can only give limited insights to why some couples separate after bariatric surgery."
In the SOS study, the surgical patients received gastric banding (n=368; 18.8%), vertical banded gastroplasty (n=1,331; 68.0%) or gastric bypass (n=259; 13.2%); controls received usual obesity care. In SOReg, all 29,234 surgical participants received gastric bypass surgery. In the SOS study, bariatric surgery was associated with increased incidence of divorce/separation compared with controls for those in a relationship (adjusted hazard ratio [aHR] = 1.28; 95% CI, 1.03-1.60; p=0.03) and increased incidence of marriage or new relationship (aHR = 2.03; 95% CI, 1.52-2.71; p<.001) in those who were unmarried or single at baseline.
In the SOReg and general population cohort, gastric bypass was associated with increased incidence of divorce compared with married control participants (aHR = 1.41; 95% CI, 1.33-1.49; p<0.001) and increased incidence of marriage in those who were unmarried at baseline (aHR = 1.35; 95% CI, 1.28-1.42; p<0.001). Within the surgery groups, changes in relationship status were more common in those with larger weight loss.
"In solid partner relationships, weight loss after bariatric surgery is probably not an issue, and in many cases the relationships can even be strengthened,” said Svensson. "However, in partner relationships that are somewhat unstable or non-functional, weight loss may increase the risk of partner separation. Unfortunately, our study can only give limited insights to why some couples separate after bariatric surgery."
Funk explained that it may be presumed that existing relationships would strengthen as bariatric patients experienced an improvement in their mental well-being and self-image. However, perhaps bariatric patients want to experience new relationships and/or maybe the partners of those patients felt less connected to the 'new person' that they were married to.
Another possibility, he said, is that previously healthy relationships suffered when things that couples may have had in common before surgery perhaps were no longer shared interests after surgery. He cautioned that this research did not establish a direct cause-and-effect relationship and the cautioned that the findings might not apply outside of Sweden.
"Many patients have told me that bariatric surgery was the best decision they've ever made, and they really do have a new outlook on life. A fresh beginning," he said. Nevertheless, he cautioned that healthcare professionals need to discuss the potential impact of bariatric surgery on their patients' relationships with others.
Read more

Dublin clinic 2/03 cancelled due to the weather circumstances.
Dear all,
Due to the weather circumstances our flight has been cancelled just now, so there will be no clinic in DUBLIN on the 2th of March. However, you can book a new appointment on our site www.belgiumsurgeryservices.com => DUBLIN = 16th or 30th of March or the 20th of April
Thanks for your understanding and sorry for any inconvenience this may cause.
Kind regards,
The BSS team
Read more

1/03 Glasgow clinic cancelled due to heavy snow
The clinic in Glasgow will be cancelled tmw due to the snow.
We will organize a new clinic on on 29/03.
Sorry for any inconvience this may cause .
Warm regards, Belgium Surgery Services
Read more
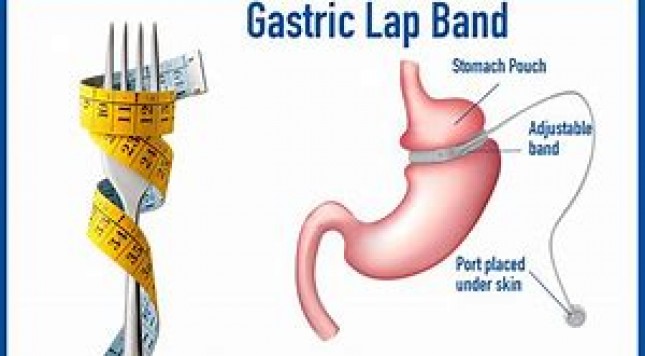
Gastric band fill for 60£ in Manchester and Birmingham
10 years celebration offer !! Belgium Surgery Services already organize for 10years gastric band aftercare clinics in the UK To celebrate this with our patients we offer gastric band fills for 60£ at our Manchester and Brimingham clinic in March and April for all gastric band patients. Appointments are limited . Book an appointment online at clinics on our website www.belgiumsurgeryservices.com or call 0032472019091
Dates for Manchester (1pm till 4pm): 8/03 and 5/04
Dates for Birmingham ( 12pm till 3pm): 22/03 and 26/04
Read more

Short-term weight loss before surgery leads to better outcomes
Patients who lose at least 8 percent of excess weight just one month before the bariatric surgery have an increased probability of losing additional in the year following surgery, according to researchers from the University of South Carolina School of Medicine, Greenville, SC. Apart from surgery, diet and weight loss before the operation may also determine how successful a person is in losing weight during the first year after the procedure.
"Currently, controversy exists for the optimal preoperative dietary optimization of patients prior to bariatric surgery,” said study co-author John David Scott, associate professor of surgery, University of South Carolina School of Medicine, Greenville, and the metabolic and bariatric surgery director of Greenville Health System (GHS), SC. “On one side, insurance policies often mandate six or 12 month weight management programmes. This mandate is in direct contrast to many bariatric surgeons, who prefer to use short-term, calorie-restricted diets several weeks prior to surgery in order to optimize outcomes."
The paper, ‘Short-Term Preoperative Weight Loss and Postoperative Outcomes in Bariatric Surgery’, published in the Journal of the American College of Surgeons, sought to determine what impact short-term pre-operative excess weight loss (EWL) has on postoperative outcomes in patients undergoing primary vertical sleeve gastrectomy (SG, n=67) or Roux-en-Y gastric bypass (RYGB, n=188).
Led by Dr Deborah A Hutcheon, a clinical nutrition specialist at GHS, the study involved 355 patients who undertook the recommended four-week low-calorie diet before surgery, between January 2014 and January 2016 at GHS. The study patients were asked to lose at least 8 percent of their excess weight by following a 1,200 calorie diet for four weeks immediately preceding their operations. For the analysis, the patients were divided into two groups based on whether they actually achieved that weight loss goal (224 patients achieved that goal, and 131 did not). Primary endpoints included percent excess weight loss (% EWL) at one, three, six and 12 months postoperatively.
Patients achieving ≥8% EWL preoperatively experienced a greater %EWL at postoperative month three (42.3±13.2% vs 36.1±10.9%, p<0.001), month six (56.0±18.1% vs 47.5±14.1%, p<0.001), and month 12 (65.1±23.3% vs 55.7±22.2%, p=0.003). Median operative duration (117 minutes vs 125 minutes; p=0.061) and mean hospital length of stay (1.8 days vs 2.1 days; p=0.006) were also less in patients achieving ≥8% EWL.
There were no significant differences in follow-up, readmission or reoperation rates were seen. Linear regression analysis revealed that patients who achieved ≥8% EWL during the four-week low-calorie diet lost 7.5% more excess weight at postoperative month 12. This finding was consistent even when other factors such as age, gender, ethnicity, and health problems including high blood pressure and diabetes were considered.

Patients who lose some excess weight prior to weight loss surgery achieve greater weight loss after surgery, and also experience shorter hospital stays and shorter procedures (Credit: American College of Surgeons)
Hutcheon explained that there is this key window of opportunity after bariatric surgery, up to 18 months, when many physical and metabolic changes occur that help facilitate weight loss.
"After that time point, patients will have to rely on diet and exercise and lifestyle management to maintain that weight loss," she said. "One of the things we often say is bariatric surgery is a tool; it's not the end-all-be-all for weight loss. So it's really about making sure this tool is used wisely and proactively by our patients and having it work most effectively in the long run.”
Scott explained that the most important aspect of this study is that it adds to the body of research data showing that it is beneficial for bariatric surgery programmes to encourage and counsel patients to follow a short-term diet or aim to achieve weight loss prior to bariatric surgery.
"Our ultimate goal was to see what makes postoperative outcomes better for our patients undergoing this lifesaving procedure," he said. "We call it the honeymoon period of bariatric surgery. After a year or year and a half, your body starts to figure out what it can and can't do, and your behaviours may change a little bit, so the odds that you are going to lose a significant amount of weight after that time period are definitely decreased. Therefore, the more weight you can lose during that honeymoon period, the better, because that effort will help establish a set point, in terms of where your steady weight is going to be further down the road."
For future investigations, the researchers hope to explore the impact that pre-surgery weight-loss programs have on longer term (more than one year) surgical outcomes.
"Ultimately, we believe that preoperative preparation for bariatric surgery should be mediated by individual surgeons taking care of their patients and this 8 percent target should not be used as a hard set point to qualify patients for bariatric surgery,” he concluded. “Because patients with obesity who weren't able to achieve that 8 percent goal still had dramatic effects in terms of how much weight they lost and comorbidity resolutions."
Read more

Short-term intragastric balloon treatment improves quality of life
Six-month treatment with intragastric balloon (IGB) was associated with significant weight loss and improvements in obese individuals with metabolic syndrome in their health-related quality of life (HRQoL), according to researchers from Federal University of Rio de Janeiro, Rio de Janeiro, Brazil. They reported that weight loss parameters were associated with short-term improvements in HRQoL, although only total fat was independently related to HRQOL perception. The paper, ‘Impact of 6 months of treatment with intragastric balloon on body fat and quality of life in obese individuals with metabolic syndrome’, published online in the journal - Health and Quality of Life Outcomes.
The aim of their study was to investigate the effect of six months of treatment with an IGB on HRQOL (including specific domains) in obese individuals with metabolic syndrome and its relationship with changes in body composition, including fat content measured by dual-energy X-ray densitometry (DXA).
The researchers recruited 50 patients from July 2011 to April 2012 and were implanted with a silicone IGB (Silimed Silicone Instrumental Médico Cirúrgico Hospitalar Ltda). The patients were subsequently followed for up to six months when the IGB was then removed.
The follow-up visits were performed at weeks 0 (baseline), eight, 16 and 24. During each visit, body weight (kg) and height (m) for calculation of their BMI was taken, as well as waist circumference (WC, cm). The body fat content (%) was evaluated at weeks 0 and 24 by DXA using a Prodigy-GE densitometer (GE Healthcare).
The authors utilised the World Health Organization Quality of Life (WHOQOL), an internationally widely used questionnaire to evaluate quality of life, translated and validated for the Brazilian population. This questionnaire evaluates and individual’s overall quality of life (question 1), general health (question 2), Physical Domain (pain, fatigue, energy, sleep, and rest), Psychological Domain (self-esteem, memory, positive and negative feelings, perceptions of body image, and appearance), Social Domain (assessment of personal relationships), and Environmental Domain (safety, financial resources, leisure time, home environment, transportation, convenience of getting information, and medical service). The WHOQOL-BREF questionnaire was applied to the study group at baseline and soon after removal of the IGB. WHOQOL-BREF was used with permission from WHO, even though the permission was obtained after the completion of the trial.
Of the 50 patients included in the protocol, 11 did not complete the study due to gastric intolerance in four, balloon rupture in five, uterus cancer in one and loss of follow-up in another one. Therefore, prospective data were analysed for 39 patients who completed the study.
Outcomes
The mean age of the cohort was 34.6±7.1 years and the mean BMI40.0±6.3. After six months of treatment with IGB, the mean reduction in weight, BMI, WC, fat free mass and total body fat analysed with DXA was 11.7±9.6kg (p<0.0001), 4.4±3.5kg/m2 (p<0.0001), 9.3±8.2 cm (p<0.0001), 3.7±4.8kg and 7.53±7.62kg (p<0.0001), respectively.
Patients who completed the study also displayed a significant improvement in almost all aspects of HRQOL measured by the WHOQOL-BREF, except the Social Domain, which presented only a trend toward significance.
The researchers then performed a correlation analysis to investigate whether the amount of weight loss would correlate with the improvement in different aspects of quality of life . The reduction in all markers of excess weight (BMI, WC, weight, and total fat [%]) was directly related to the improvement in general aspects of HRQOL (questions 1 and 2 of the WHOQOL-BREF).
These results were not observed for the specific domain of the questionnaires. For the Physical Domain, only the reduction in WC was associated with the improvement. For the Environmental Domain, only the reduction in body fat measured by DXA correlated with the improvement in the scores. Among all domains of the WHOQOL-BREF, Physicological did not meet the requirements.
Therefore, the authors stress that the results of their study are not applicable to patients with psychiatric syndromes and they state additional studies are necessary to clarify the impact of IGB in this specific population.
Multiple linear regression was used to identify which variables (anthropometric and DXA) independently correlated with the improvements in quality of life. ‘Question 1’ and ‘Question 2’ were used as the dependent variable and three different factors indicative of weight excess as independent variables (i.e., BMI, WC, fat free mass and total fat [%]).
Both models were also adjusted for age and gender. After regression, only total fat (%) remained independently related to question 1 (p=0.047). On the other hand, no variable (i.e. BMI, WC, and total fat [%]) reached statistical significance after regression for Question 2.
“Our study demonstrated that weight loss, particularly the reduction in body fat, was associated with improvement in general HRQOL,” the authors write. “These results strongly suggest that, although several different mechanisms may be proposed to explain the improvement in specific aspects of HRQoL after rapid weight loss, the reduction in body fat seems to be one of the main determinant in this improvement.”
Read more
UK: Public do not recognise link between obesity and cancer
The majority of people in the United Kingdom do not understand the connection between weight issues and cancer, according to a study by Cancer Research UK. Despite the fact that 63% of the English and 67% of the Scottish adult population is overweight, only 25.4% of this population listed cancer as a health issue related to being overweight when asked an unprompted question.
The study, ‘Public awareness and healthcare professional advice for obesity as a risk factor for cancer in the UK: a cross-sectional survey’, published in the Journal of Public Health, after surveyed 3,293 adults, taken as representative of the UK population, researchers found that only a quarter of respondents were aware of the link between obesity and cancer
"We're very concerned that most people simply don't connect cancer with obesity. This study shows that only one in four know that excess weight increases the risk of cancer so we need to make the link very clear. This may go some way towards tackling the obesity epidemic which all too often begins in childhood,” said Dr Jyotsna Vohra from Cancer Research UK and study co-author. "Our study also showed that GPs aren't discussing weight with patients who are too heavy as often as they might. GPs have very little time during their appointments and should have more support to introduce sensitive issues such as obesity, with patients."
There study found that there were also several misconceptions about cancer types linked to obesity. Researchers found greater levels of awareness about cancers of the digestive system organs, than for those of the reproductive organs, such as womb or breast.
The study's authors also examined the impact of respondents' socio-economic background and found that those in a lower income group were more likely to be overweight or obese and were less aware of the link between weight issues and cancer. Modelled projections show obesity trends will increase by 2035 and the gap between the highest and lowest income groups will widen further.
Although there are currently several healthcare initiatives to address obesity issues, the study found that not all participants had seen a healthcare professional in the last 12 months. Of those who had, only 17.4% had received advice about their weight, despite 48.4% being overweight.
Those who received advice were mainly instructed on how to lose weight, rather than given information about the range of health issues associated with being overweight or obese.
“Cancer is not at the forefront of people’s minds when considering health conditions associated with overweight or obesity,” the authors concluded. “Socio-economic disparities exist in health knowledge across the UK population, with adults from more affluent groups being most aware. Healthcare professionals are uniquely positioned to provide advice about weight, but opportunities for intervention are currently under-utilised in healthcare settings
Read more

obesity and cosmetic clinic LONDON 2017-2018
Dear Custumors,
Our new office at Devonshire place 35 in London is ready . We've moved to the first floor in close corporation with The Harley Street Dermatologic Clinic to improve our services. The clinic will be open every other Friday with exception of Friday 27/10 . We will organize a clinic on Wednesday 25/10 from 10am till 2pm .
Looking forward to welcome you all at our new facilities in the future.
Read more

Cost-effective bariatric surgery under-utilised in the UK
A keynote session at the 22nd World Congress of IFSO (International Federation for the Surgery of Obesity and Metabolic Disorders) in London, has called for an increase in bariatric surgery in the number of procedures in the UK, as procedure numbers revealed the UK is behind other countries, including near neighbours in Europe.
More than 2,000 experts from around the world have gathered in the capital for the World Congress to share expertise on tackling the global obesity crisis, with the British Obesity and Metabolic Surgery Society (BOMSS) as the host association.
As part of the Congress, a panel of UK clinicians, scientists and policy makers attended a special session on Friday 1st September to debate why more surgery is not being commissioned in the UK against a background of successful surgical interventions and rising obesity levels. They questioned why a treatment that is both medically- and cost-effective is under-utilised, and asked whether barriers to access include social stigma along with misconceptions about how people become obese and then how difficult it is to lose excess weight.
The UK ranks 13th out of 17 in a table of European countries which measure bariatric surgery by number; it is 6th out of eight G8 countries and 4th out of G8 countries ranked by size of economy.
In France, which has a similar population size to the UK, more than 37,000 surgeries are carried out each year, compared to around 5,000 in the UK. Belgium (population 11.3 million) performs approximately 12,000 surgeries and Sweden (population 9.9 million) more than 7,000 surgeries a year. Italy, a little smaller than the UK population at 60.6 million, carries out more than 8,000 surgeries a year.

Mr Richard Welbourn
“The annual volume of bariatric/metabolic procedures is five to ten-fold lower when compared to other European countries with similar population sizes and disease prevalence,” said Mr Richard Welbourn, Consultant Bariatric Surgeon at Musgrove Park Hospital, Taunton and President of IFSO 2017. “Increasing surgery rates would have major benefits for patient health and reduce direct healthcare expenditure within two years.”
Headline figures from the National Bariatric Surgery Registry (NBSR), which collects information on bariatric surgery, shows that bariatric surgeons in the UK are highly successful at helping people control their weight - even though patients are increasingly overweight and have more health complications at the point of surgery, including diabetes, arthritis, depression and sleep apnoea.
But despite these successful results - and the fact that bariatric surgery has been judged as very safe with a mortality rate of less than 1 in 1,000 according to latest HES figures - many people in the UK find it difficult to access surgical treatment for obesity.
A freedom of information request published earlier in 2017 revealed that some Clinical Commissioning Groups either require patients to stop smoking or to have a BMI>50, despite NHS England and the National Institute for Health and Care Excellence (NICE) guidance stating bariatric surgery is cost-effective and should be considered for patients with BMI>35 with an obesity-related disease co-morbidity (such as such as high blood pressure, high cholesterol levels, osteoarthritis, depression) or a BMI>40 without a related disease.
In patients with Type 2 diabetes, both NICE recommendations and international guidelines - endorsed by over 50 organisations including Diabetes UK and all relevant British professional societies - advise considering metabolic surgery for patients with inadequately controlled diabetes and a BMI>30 (or 27 for patients of Asian descent).
The NBSR - which will next report fully in early 2018 - has data on 18,528 operations which were performed between 2015 and 2017, and shows that UK surgeons are operating on an increasing sick and older population. Of the people treated, the average BMI47.2, (almost twice the weight people should be for their height). Some 65.4% of men and 64.4% of women had what is known as functional impairment - eg, they couldn’t climb three flights of stairs without resting. One year after surgery, well over half of those patients (58.3%) no longer had any functional impairment.
The results for diabetes resolution are startling and could offer a solution to the increasing cost burden on the NHS of treating the condition. Some 51.6% of patients with Type 2 diabetes at the point of surgery showed no indication of diabetes one year after surgery, coming off costly diabetic medications. NBSR results are consistent with a large body of evidence including 12 randomised clinical trials showing that surgery is more effective than other available treatment options in controlling diabetes in obese patients.
“The UK data is overwhelming - surgery makes a difference to people’s health and we want commissioners to acknowledge this and act accordingly,” said Mr Marco Adamo, Consultant Surgeon at UCH and Chair of the NBSR. “Severe and complex obesity is a serious, life-long condition associated with many major medical conditions, the cost of which threatens to bankrupt the NHS.”
Despite its proven health benefits and cost-effectiveness, surgical treatment for obesity or diabetes remain largely underutilised in the UK. 2.6 million British people would be eligible for surgery under guidelines covering BMI and co-morbidities.

Professor Francesco Rubino
“When clinical evidence of efficacy and safety, high cost-effectiveness, NICE guidelines and international consensus by all relevant professional organisations are not sufficient to ensure appropriate access to bariatric/metabolic surgery, then it becomes clear that misconceptions and the stigma of obesity are the main barriers,” said Professor Francesco Rubino, Chair of Metabolic and Bariatric Surgery at King’s College London. “Whenever possible, prevention is obviously better than cure. But for people who are morbidly obese or have already developed diabetes, prevention is obviously no longer an option. Focusing on prevention alone and denying access to treatment to the many patients already suffering from clinically severe obesity or Type 2 diabetes is a sure way to inflict damage to patients and to the healthcare system at the same time.”
Read more

MGB and one-anastomosis gastric bypass are on the rise
The MGB-OAGB 4th Annual Consensus Conference was held in Naples, Italy July 3-4, 2017 under the superb organisation of Professor Mario Musella, at a beautiful site on the Mediterranean seaside. The meeting was attended by 169 experienced surgeons from bariatric teams in 29 countries, where important studies were presented and discussed.

This article was authored by Mervyn Deitel, MD, SFASMBS, FACN, Director MGB-OAGB Club, Toronto, Canada
A French group reviewed their 2,014 MGBs; abscesses had occurred in 2.2% and were treated by endoscopic or percutaneous drainage, with no mortality. Methylene blue test has been important for operative detection of leaks. Revision for GE bile reflux or malnutrition was rarely necessary in the long-term. The operations were highly effective for excess weight loss. Studies suggested that the length of the bypassed limb may only influence weight loss in the early months after surgery. Bypasses of 150-250 cm were performed, depending on BMI and sociocultural conditions, but with the longer bypasses, total bowel length should be measured to be certain that 300 cm of common limb is left distally.

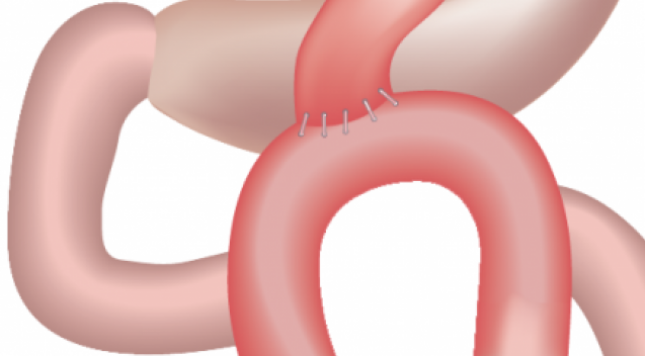
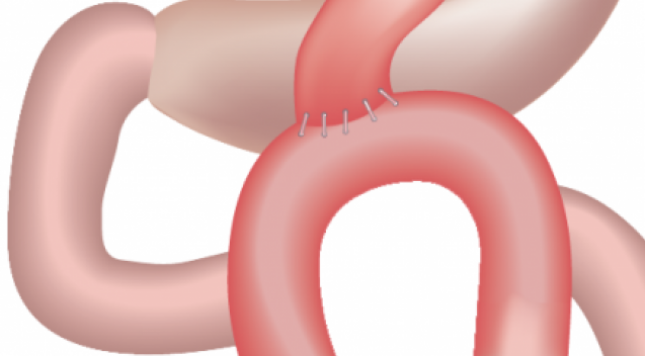
Figure 1: MGB with a long gastric pouch, starting from below the crow’s foot, and going proximally to the left of the angle of His. An anterior wide gastrojejunostomy is constructed 180-200 cm distal to Treitz’ ligament.
MGB or OAGB was performed safely as both a primary operation or a revision for failed gastric banding or sleeve gastrectomy (SG). Improvement in quality of life and co-morbidities resulted, with resolution of type 2 diabetes in >95%.
Cady of Paris, with 3,500 cases (using a 175-200 cm bypass limb), found that under-nutrition occurred in 1.5%, and if there is no quick result from replenishment, reversal is necessary to avoid death. The French group from Cornevarrieu-Toulouse reported that in their series of 2,400 patients with a 150-cm biliary limb, had 0.04% severe malnutrition (only 1 patient) requiring reversal. Weight loss after MGB-OAGB depends mainly on malabsorption. Malnutrition in patients in India (where 50% are vegetarian) is avoided by a bypass no greater than 200 cm and proper diet.

Figure 2: OAGB with long, narrow gastric pouch (15-18 cm) and an antecolic antegastric latero-lateral anastomosis between pouch and afferent enteric loop which is suspended ~8-10 cm above the anastomosis through an initial continuous suture which secures the afferent limb to the gastric pouch’s staple-line and with final fixation of the loop’s apex to the excluded stomach. Biliopancreatic limb averages 250-350 cm.
With the usual MGB gastric channel constructed 2-3 cm distal to the crow’s foot, bile GE reflux was negligible. The Kazakhstan group found that a longer gastric pouch significantly reduced postop bile reflux. Tolone’s group from Naples (S Tolone SOARD 2016), using multiple scientific studies, confirmed that GE reflux does not occur after MGB (unlike after SG which maintains the pylorus).
Carbajo of Spain and Luque-de-Leon of Mexico presented their outcomes from 2,850 OAGBs since 2002, with negligible bile reflux, marginal ulcer in <1%, and EWL and EBMIL >75%. Again, the OAGB was an excellent rescue after other failed operations. Long-term %EWL and co-morbidity resolution after OAGB were similar to the best results obtained with more aggressive and complex operations.
The importance of differentiating type 1 (auto-immune) diabetes (T1D) in the adult from type 2 diabetes was emphasised. Obesity can occur in type 1 if the patient takes excessive insulin, becomes hypoglycaemic, and then has to eat more (a vicious cycle). This can be controlled by dietary surveillance; if not, bariatric surgery for obese T1D will decrease weight, lower HbA1c, and lower insulin requirement. However, the T1D patient will always require insulin.
Unlike following other bariatric operations, carcinoma in the gastric channel or esophagus has not occurred. Some workers are performing robotic MGB, and note speed and technical ease.
A number of long-term studies comparing MGB-OAGB with SG and RYGB were presented. SG was followed by occasional serious high leaks, GE reflux, Barrett’s esophagus, and weight regain. Most MGB and OAGB surgeons had previously performed RYGB for many years. RYGB took longer to perform, was more complex, had longer learning curve, more marginal ulcers, increased internal hernias and bowel obstruction, more hypoglycemia, late weight regain and more difficulty to revise.
In comparison, MGB was relatively simple, rapid, safe, and had greater elevation of GLP-1, durable weight loss, ease of revision and reversal, and resolved GERD. With both RYGB and MGB, watch for iron deficiency anemia and hypoalbuminemia.
In many countries outside USA, MGB and OAGB have become the most common bypass operation for bariatric patients.
Read more
Gastric band aftercare London
Dear patients, we will organize a clinic in London on Friday 28/07 between 9am and 1pm.
For appointments please book online on our website.
Have a nice summer and we 're looking forward to see you again soon.
Read more
OAGB – the long-term outcomes from 1,200 procedures
Laparoscopic one-anastomosis gastric bypass (OAGB) is a safe and effective procedure, that reduces difficulty, operating time and early and late complications associated roux-en-Y gastric bypass, according to the authors of a study from the Centre of Excellence for the Study and Treatment of Obesity and Diabetes, Valladolid, Spain. They also note that long-term weight loss, resolution of comorbidities, and degree of satisfaction “are similar to results obtained with more aggressive and complex techniques. It is currently a robust and powerful alternative in bariatric surgery.”
The paper, ‘Laparoscopic One-Anastomosis Gastric Bypass: Technique, Results, and Long-Term Follow-Up in 1200 Patients’, published in Obesity Surgery, sought to evaluate experience and long-term follow-up (FU) in a large cohort of patients with morbid obesity who underwent laparoscopic OAGB at a single institution. The retrospective review of a prospectively maintained database included 1,200 consecutive patients from July 2002 to October 2008, and included follow up from six to 12 years.
Outcomes
There were 744 female (62 %) and 456 male (38 %) patients with a mean age of 43 years (range, 12–74). Mean pre-operative BMI46 (range, 33–86) and mean preoperative excess weight was 65kg (range, 34–220). The cohort included 697 patients (58 %) with no previous or simultaneous abdominal operations (subgroup 1). Another 273 (23 %) had had prior open abdominal operations and thus required adhesiolysis of variable complexity, and a total of 203 (17 %) had abdominal operations performed simultaneously, particularly gallbladder removal and/or hiatal or ventral hernia repairs (subgroup 2). Finally, in 27 (2 %), laparoscopic OAGB was performed as a revision of other (failed) bariatric procedures (subgroup 3) including previous laparoscopic gastric bands (n=13), as well as open vertical banded gastroplasties (n=14).
Intraoperative complications requiring conversion to an open approach occurred in four patients (0.3 %). Early major complications requiring reoperations occurred in 16 patients (1.3 %) and included intra-abdominal bleeding (9), leaks (3), and early small bowel obstruction (2). Late complications included 6 stomal stenosis (0.5 %) 6 (0.5 %) anastomotic or marginal ulcers (MU).
The 30-day readmission rate was 0.8 % (10 patients). Late readmissions were required in 13 patients (1 %) for stomal stenosis (6), GI bleeding due to MU (5), and malnourishment (2). Two patients died in this series (0.16 %); both had super-obesity, multiple comorbidities and risk factors. One suffered a pulmonary thromboembolism 3 days after BS (without warning symptoms or additional postoperative complications). The other suffered gastric wall necrosis, was re-operated on, and developed refractory nosocomial pneumonia. Both deaths occurred during the initial part of the series, and there were no other casualties in >1000 patients operated on thereafter.
Pre-operative nutritional deficits were found in some patients including iron (∼10 %), vitamin D (∼15 %), and calcium (∼4 %). After OAGB, a few patients developed excessive weight loss and/or nutrient deficits (usually within the first 2–3 postoperative years). A total of 14 patients (1.2 %) required further treatment for hypoalbuminemia; all received high-protein enteral supplements and pancreatic enzymes. Iron deficiency was rather common, especially in fertile women with copious menstrual bleeding and up to one third required oral supplements beyond the expected time for intestinal adaptation, and 15 patients (1.3 %) required parenteral iron.
Among liposoluble vitamins, vitamin D insufficiency was present in more than half of patients at three years and one third in the long term; this required continuous supplementation in ∼20 % of them. Longer supplementation was also needed for vitamins A and K in ∼3 and 0.5 %, respectively.
Patients lost a mean of ∼15–20 kg in the first month and ∼30–40 kg in the first trimester. The number and percentage of patients followed up at each time interval are included; only from 13 % (at 6 years) to 30 % (at 12 years) of the cumulative number of patients were lost for follow-up. Substantial weight loss was documented for most patients; through time, there was a slight weight increase in a few, which was not clinically relevant. Therefore, the authors stated that excess weight loss was maintained in most of these patients and according to Reinhold’s classification their results ranged from good (EWL >50 %) to excellent (EWL >75 %), and a long-term successful treatment (EWL >50 %) was achieved in almost all patients.
Severe metabolic comorbidities such as type II diabetes mellitus, insulin resistance, hypertension, and sleep apnoea either totally resolved or substantially improved, most from the first day after surgery (Table 1). Remission was also demonstrated in most patients for other metabolic conditions like hyperlipidaemia and liver steatosis when the first biochemical tests were ordered at the 3rd postoperative month. Interestingly, 53 % of patients had gastroesophageal reflux disease (GERD) of some degree before surgery, and all were relieved after the operation.

Table 1: Outcomes of one-anastomosis gastric bypass (OAGB) on comorbid conditions in 1200 morbidly obese patients
“We call again on the various bariatric teams that are performing the original MGB or our modified version, the OAGB, to aid in the dissemination and acceptance of this procedure by presenting and publishing their experiences and standardising the name (to MGB/OAGB), in order for all of us to be recognized as a whole,” the authors write. “Now that many of its controversies are being surpassed and the bariatric surgical community is accepting the procedure as a rational alternative in the bariatric repertoire, we should make all efforts in order to conciliate in regard to the name, avoid new disagreements, and work towards making MGB/OAGB mainstream in obesity and metabolic surgery.”
“Concerns regarding bile reflux and its potential consequences currently seem unsubstantiated but await studies with even longer-term outcomes,” the authors conclude. “So far, development of subsequent cancer has not been reported. Long-term substantial EWL, remission of comorbidities through its metabolic benefits, and degree of satisfaction are similar to the best results obtained with more aggressive and complex operations. OAGB is a safe and effective powerful alternative which is slowly (but surely) becoming mainstream in bariatric surgery.”
The article was edited from the original article, under the Creative Commons license.
To access this article, please click here
Read more
gastric band DUBLIN
Due to the number of weightloss surgery patients we've have in Ireland we will now organize 3 times a moth aftercare clinics in Dublin.
Price for gastric band fill or defill will be 120€.
Price for initial consultattion will be 30€.
All previos patienst from the hospital group and patients who didn't have the surgerty done with oruselves are more the welcome for follow up and advice.
Kind regards, BSS team
Read more

Post-op dumping syndromes
Acarbose, a glucosidase inhibitor that slows carbohydrate digestion, has been found to result in complete remission of dumping syndrome (DS) in most subjects and substantially decreased the frequency and intensity of both early and late DS events. The study researchers from Brazil, stated that previous studies have been reported an associated acarbose with the remission of late dumping, although not early dumping. Therefore, they wanted to evaluate the role of acarbose in dumping syndrome prevention and treatment and in resistive exercises resistance in bariatric subjects.
The paper, ‘Acarbose promotes remission of both early and late dumping syndromes in post-bariatric patients’, published by Dovepress, included patients who had previously undergone Roux-en-Y gastric bypass surgery and had achieved body weight goal (BMI<27 for men and <25 for women), had a confirmed diagnosis of DS and were refractory to diet recommendations. Inclusion criteria were the complete adherence to an isocaloric (calculated by indirect calorimetry) and high protein (1.5–1.8 g/kg/day) diet plan, proposed resistive exercises (frequency, intensity, and exercise prescription varied among individuals), and age between 18 and 80 years. Patients who lacked regular follow-up were excluded.
Fifty milligrams of acarbose was orally administered 4–5 times a day before meals for 6 months. For those patients who presented with severe flatulence, 120mg simethicone (b.i.d.) was additionally prescribed. The dose of 50mg before meals has been extensively studied and standardised,14–16 whereas the addition of simethicone was thought to attenuate the most important adverse effects of acarbose use (abdominal cramps, bloating, and flatulence).
A total of 25 subjects (13 men and 12 women; mean age, 37.2 years) were regularly followed up. None of the patients withdrew or missed doses. Among these, seven presented with severe flatulence and one patient showed persistent flatulence despite simethicone prescription. None of the subjects stopped acarbose use owing to side effects. Significant improvements (Table 1) were seen in all analysed parameters: 1) mean number of early DS episodes per week (2.18–0.31; 85.8% reduction; p<0.001), 2) mean number of late DS episodes per week (2.79–0.12; 95.7% reduction; p<0.001), 3) self-referred intensity of each episode (6.1–1.65; 73.0% reduction; p<0.001), 4) Sigstad’s score (2.36–0.32; 86.4% reduction; p<0.001), and 5) ability to perform resistive exercises (3.03–7.12; 135.0% improvement; p<0.001). Improvements were observed from the beginning of the use of acarbose and persisted throughout the six months of therapy.

Table 1: Summary of the results
Complete remission of DS (except during exercises) was observed in 21 patients (84% of analyzed subjects), which persisted throughout the 6 months of acarbose use in all 21 subjects.
The authors acknowledge that a limitation of the study is that they did not include a control group to study the possible placebo effect of acarbose, although it is unlikely that the observed improvements are due to placebo effect.
“Further prospective randomised placebo-controlled double-blind clinical trials with monitoring of vital signs and glucose should be performed in order to confirm our findings,” the authors conclude. “Until then, acarbose may be treated as an option for refractory DS subjects.”
The article was edited from the original article, under the Creative Commons license.
Read more
Bariatric Surgery Can Help People Keep Weight Off Long Term
It really hit Terry White eight years ago when he was at the mall with his wife. He was out of breath every few minutes and had to sit down. "My wife told me I had to get to the gym and lose weight," he says.
He had dieted most of his life. "I've probably lost 1,000 pounds over the years," says White, a realtor in North Myrtle Beach, N.C. But he put most of it back on.
By age 59, he knew he was headed for disaster; he weighed 387 pounds at just 5 foot 6. With encouragement from a friend, he headed to Duke University Medical Center in Durham where he had gastric bypass surgery. It reduced his stomach to about the size of an egg so his body absorbed fewer calories and fat from food.
The weight just fell off, he says. He didn't feel deprived. He just didn't want to eat that much. In seven months he'd lost 200 pounds. That was eight years ago. He's gained back a bit, but not much. It turns out his success isn't unique.
Article continues after sponsorship
Researchers with the Durham Veterans Affairs Medical Center in North Carolina recently tracked the progress of 1,787 veterans who underwent gastric bypass surgery. They found that one year after surgery patients lost 98 pounds on average. Ten years later they gained back only about 7 pounds.
Earlier studies have tracked gastric bypass patients for relatively short periods of time, about 1 to 3 years. That has led to the assumption that most people who have gastric bypass surgery will eventually regain the weight.
This study, published online on August 31 in JAMA Surgery, is one of the largest and longest to evaluate the surgery's effects on weight loss. It also did a better job than many studies at follow-up, with 82 percent of participants staying in the study for 10 years.
Researcher Matthew Maciejewski at the Duke University School of Medicine collaborated with Dr. David Arterburn, a senior investigator at Group Health Research Institute in Seattle, in analyzing the data. They expected to see gradual weight gain over 10 years, with some patients gaining back everything they lost.
But they were pleasantly surprised. Patients regained a small amount of weight in the first few years after surgery, but then they "actually plateaued and maintained their weight loss and even lost a little more weight over the next few years," says Arterburn. Just 3 percent of the study participants gained most or all of the weight back in 10 years.
He says the surgery likely interferes with the body's natural defense to less food: a slowdown in metabolism. This is what dooms so many dieters. The study compared the 1,787 veterans who had the surgery to 5,305 equally obese patients who did not have surgery. For the nonsurgical patients, their weight after 10 years essentially stayed the same.
Arterburn says bariatric surgery seems to change how the brain perceives hunger. "Even though they're taking in a whole lot less calories than they were before, they don't feel a constant urge to eat, and it's not just a reduction in the size of the stomach. They don't feel hungry in between meals."
This is exactly what happened to Terry White, who is now 67. He no longer falls asleep all the time. He walks and jogs about 5 miles daily. He and his wife Wanda are planning to charter a boat in the West Indies to celebrate their upcoming 50th anniversary. He says it's been an "unreal" and extraordinary change in his quality of life.
Researcher Maciejewski says the findings of the study provide evidence that bariatric surgery can be highly effective for severely obese patients. He says further research is needed to look at postsurgical complications and how the experience affects long term mental health.
Read more

gastric band aftercare Dublin : 2017
Dear all,
Every second week we will organize gastric band afterrcare clinics at the Meridain clinic at Clarehaal shopping centre.
All patients are welcome between 9am and 4pm . Emergency defills are possible at anytime if needed.
For appointment please book online at clinics or call 0032472019091.
The dates for gastricband fills 2017 are available on our website.
Read more
Gastric band Aftercare : the key to your succesfull weight loss.
Apollo completes Lap-Band post-approval HERO study

At the five-years visit, mean weight loss from baseline to five years was 51lbs (23.1kgs) and mean BMI reduction was 8.3
The HERO Study had an explant rate of 8.74%, which met the success criteria for the primary endpoint

Monday, November 7, 2016 - 11:13
Owen Haskins - Editor in chief, Bariatric News
Apollo Endosurgery has announced the completion of the Lap-Band AP Adjustable Gastric Band HERO (Helping Evaluate Reduction in Obesity) post-approval study. This study was initiated in June 2009 as part of the FDA’s condition of approval for the Lap-Band System in the US.
The HERO Study was a multi-centre, prospective, non-randomised study of 652 enrolled patients in the US and Canada. Patients were required to have either a baseline body mass index (BMI) of at least 40, or a BMI of at least 35 with one or more severe co-morbid conditions, or be at least 100 pounds (45.4kg) over their estimated ideal weight.
Patients had an average age of 44.4 years (ranging from 18 to 76) with an average baseline weight of 280.7lbs. (127.3kg) and an average BMI of 45.4. Females represented 79.3% of the patients.
The primary endpoint was the percentage of patients who experienced the removal of the Lap-Band AP System within or at five years from the date of surgery (the explant rate). The successful primary endpoint, as defined in this study, was a significantly lower explant rate than the 39.4% found in initial Lap-Band System clinical studies (cited in the Lap-Band System Directions for Use). The HERO Study had an explant rate of 8.74%, which met the success criteria for the primary endpoint.

John Olsofka
“This study demonstrates that continued patient interaction and adherence to good Lap-Band aftercare principles by the surgeon’s practice will produce an effective, safe, and durable outcome for patients who suffer from obesity,” said Dr John Olsofka, Louisville Surgical Associates, KY, and one of the lead investigators of the study.
The average percent total body weight loss (TBWL) for the enrolled patients increased progressively within the first year of Lap-Band AP placement, increasing from an average of 10.3% at three months to 17% TBWL at the end of the first year. At the five-year visit, the average TBWL was 18%. Mean weight loss from baseline to five years was 51lbs (23.1kg) and mean BMI reduction was 8.3.

Vincent Lusco
“As the HERO Study shows, the key to success with Lap-Band is for it to be viewed as a therapy as much as a surgical procedure,” said Dr Vincent Lusco, another lead investigator, also from Louisville Surgical Associates. “When delivered by bariatric surgeons who have the required aftercare programme, laparoscopic adjustable gastric banding with the Lap-Band is an excellent alternative for patients looking to gain control over obesity.”
“The results demonstrated in the HERO Study are consistent with what we see at bariatric practices who have appropriately tailored and prescriptive follow-up programs for their patients,” said Todd Newton, CEO of Apollo Endosurgery. “We remain confident that the Lap-Band System is a great option for patients seeking medically-relevant weight loss results at bariatric practices where these tailored follow-up programs are in place.”
Read more

Ireland: Mini gastric bypass Belgium today on the Shaun Doherty radio show
2 of our Irish patients shared their experience about coming over to Belgium for weightloss surgery with Dr Chris Debruyne and Belgium surgery services at the Shaun Doherty radio show.
Listen from minute 101:30 to their amazing story on the link bellow:http://www.highlandradio.com/2016/10/27/shaun-doherty-show-listen-back-to-thursdays-show/
.
Read more

Diabetes type 2: How gastric surgery can 'cure' patients
Thousands of patients with type 2 diabetes are being denied the chance of life-saving surgery because they do not fit strict NHS guidelines on weight.
Around 3.6m people in the UK suffer from type 2 diabetes, which costs the NHS up to £10bn a year to treat.
A leading bariatric surgeon told Inside Out surgery was "the closest thing to a cure" and should be used more often.
Only type 2 patients with a BMI over 30 are currently eligible under obesity guidelines.
At least 15% of sufferers are of normal weight and therefore don't qualify for operations like gastric bypasses on the NHS.
Of those who do meet the criteria - less than 1% access surgery.
The Chair of Bariatric and Metabolic Surgery at Kings College, Professor Francesco Rubino, has been researching the effects of bariatric surgery on type 2 diabetes for 15 years.
"I don't think this is seen as a lifesaving operation as it is," he told the BBC.
"The biggest barrier we have is primarily one of stigma against obesity. The vast majority of the public believes this is a cosmetic intervention and unfortunately many physicians think the same way."
'A foreign parameter'
Professor Rubino said operations involving the manipulation of the stomach or intestine do not just help people lose weight - they also alter hormones in the gut, which in turn influences insulin production.
"More than 50% of people with type 2 diabetes can enjoy long term remission. Another 30 or 40% enjoy a major improvement," he added.
How does it work?
Out of media player. Press enter to return or tab to continue.
Media captionThis video explains how a gastric bypass is carried out
Bariatric surgery refers to a set of operations carried out with the primary intention of helping people who are morbidly obese lose weight.
The two most common types of weight loss surgery are:
Gastric band, where a band is used to reduce the size of the stomach so a smaller amount of food is required to make someone feel full.
Gastric bypass, where the digestive system is re-routed past most of the stomach so less food is digested to make someone feel full.
Professor Rubino said the use of bariatric surgery was currently "shaped around weight loss", with remission from diabetes seen as a by-product.
Instead, he said, it should be offered as a "standard treatment" for type 2 patients, who are not responding to dietary or pharmaceutical intervention, regardless of BMI.
He wants to see guidelines from the National Institute for Health Care and Excellence (NICE) updated to reflect this.
"Diabetes care practitioners don't use BMI to decide whether you go on one medication or another. So why should surgery be regulated by a parameter that is foreign to the management of diabetes?
"In patients who have done everything possible - what is the point of not offering it, just because their BMI does not fit the criteria that we have arbitrarily introduced for the treatment of obesity?"
Professor Rubino said type 2 diabetes was often "dismissed as something that can be easily managed through diet and exercise".
"When diabetes is fully developed it becomes a serious disease and many patients - 50% or more - are not able to control it, no matter how many medications they take," he added.
He said each bariatric operation costs £6,000, making it "one of the most cost effective interventions in medicine at the moment".
'I signed up to Dignitas'
 Image caption Barbara Gratton from Yorkshire has normal blood sugar levels post surgery
Image caption Barbara Gratton from Yorkshire has normal blood sugar levels post surgery
Barbara Gratton, 53, suffered with type 2 Diabetes for nearly 20 years.
It was caused by a genetic disorder called Familial Partial Lipodystrophy, which prevents her body from properly storing fat and caused her pancreas to malfunction.
Mrs Gratton's low weight meant she did not quality for bariatric surgery under the current obesity guidelines set by NICE.
"My systems had become resistant to any kind of medication. So I was looking at the co-morbidities - heart failure, stroke, blindness," she said.
Mrs Gratton was so worried about her future she signed up to Dignitas, an assisted suicide organisation.
What is Type 2 diabetes?
Diabetes is a condition that causes a person's blood sugar to become too high.
Type 1 can develop at any age, but often begins in childhood. It is not related to diet or lifestyle.
Type 2 is far more common. It is usually seen in adults and can be associated with obesity. It can lead to serious complications, including kidney failure, blindness and heart disease.
It's the most common cause of vision loss and blindness in people of working age.
After a two year battle with "NHS bureaucracy" she was eventually offered surgery - but at that point she had already signed up for private treatment under Professor Rubino.
She underwent a bypass operation at Kings College Hospital on 5 September and within days she was off the insulin needed to control her blood sugar levels.
"It allows me to have a normal life, even with my underlying condition.
"If you have type 2 diabetes at these lower BMIs - £6,000 will get it done and reduce liver cancer and strokes."
'Not big enough'
Some 6,000 bariatric operations are carried out in the UK every year. Around a quarter of these patients have type 2 diabetes.
 Image caption Mr Benge's diabetes was impacting his quality of life and making him depressed
Image caption Mr Benge's diabetes was impacting his quality of life and making him depressed
Britain lags behind other European countries, where around 50,000 bariatric operations are carried out every year.
Even those who fall within the weight parameters set by NICE can struggle to gain access on the NHS.
David Benge, 56, from Hastings, recently had gastric bypass at Kings. He was initially told he was not "big enough" despite having a BMI of 36.
"From GP level they were saying it's not enough for us to refer you," he said.
"So there was a bit of pushing... at the time to get me referred, which they did in the end."
Mr Benge's blood sugar levels also dropped dramatically in the days after surgery.
Director of the Centre for Guidelines at NICE, Professor Mark Baker, said there might be scope to extend obesity and diabetes' guidelines in the future.
"There is very little doubt that people with type 2 diabetes - and at any level of weight - can see their glucose control improved by bypass surgery," he added.
"It is an effective treatment and we'd like it to be more widely available. But there are other priorities in diabetes and there is a limited budget."
An NHS England spokesperson said: "Bariatric surgery should only be considered for severe obesity where other approaches have not been successful."
Read more

13 stone weightloss after gastric band surgery
Wicklow Rose who underwent gastric band surgery: 'I lost 13 stone following the surgery, but I found that I just wasn't that happy still'
Jane Harrison (26) has overcome body shamers and low self-esteem to become this year's Wicklow Rose in the Rose of Tralee. She tells our reporter why a healthy mind is just as important as a healthy body
Joanna Kiernan Twitter
Published 27/06/2016 | 02:30
 5Wicklow Rose Jane Harrison lost 13 stone after gastric band surgery
5Wicklow Rose Jane Harrison lost 13 stone after gastric band surgery
Jane Harrison will compete in this year's Rose of Tralee. Photo: Colin O'Riordan.
Wicklow Rose Jane Harrison (26) had battled with her weight most of her life. In February 2011, however, aged 21 and weighing 23 stone, she had gastric band surgery to assist her weight-loss.
"I feel like there is a huge stigma to weight-loss surgery. It is something that scares me to talk about, but at the same time I would like people to know that it is definitely not the easy way out," Jane says.
"I remember lying there in pain thinking I would never put myself through it again. It is definitely a wake-up call. There are thousands of people getting it done every year and many people are afraid to say it, in case they might be looked at as cheaters almost.
"It was the hardest route I have tried and I tried them all; I tried liquid diets, I tried dietitians, everything."

Jane's weight began to decrease rapidly in the year-and-a-half that followed her surgery, but her mindset remained the same, causing her self-esteem to plummet even further.
"At that point I still had not dealt with the real problems that had led to my weight gain," Jane explains. "So I lost 13 stone, but had yet to acknowledge that the overeating and the unhealthy lifestyle were caused by my self-esteem issues.
"I lost the weight and then became obsessed with trying to maintain it; I was going to external people and things to get my happiness because overeating was no longer an option for me.
"You just turn those destructive habits to something else unless you really deal with it," Jane adds. "I felt so defeated when I managed to get down to 10 stone at one point and would go out and get a few compliments, but I would go home and still feel empty."
Over time, Jane learned to address the self-esteem issues she had developed in childhood: "From the age of 12 I was going to nutritionists and child dietitians. So my weight was an issue throughout my entire childhood."
"My parents were my backbone growing up and they knew I just couldn't get my overeating under control even throughout my teens and they helped me try every angle.
 55Wicklow Rose Jane Harrison lost 13 stone after gastric band surgery
55Wicklow Rose Jane Harrison lost 13 stone after gastric band surgery
"I went on a liquid diet once for 16 weeks and I lost about four stone in six weeks, but I put it back on in double, everything was just short term because there was something not right underneath it all.
"From about maybe 13, when you start going out to discos and everybody is wearing fab clothes that you cannot, that is when you start to realise 'well maybe I am a bit different,' but I have always had the best group of friends and family around me so I was never bullied as such, but you would hear comments and jabs."
Being overweight for such a long period left Jane feeling like she was still the overweight person in every room.
"I lost quite a lot of the weight following the surgery, but I found that I just wasn't that happy still," Jane explains. "I thought that someday, I was just going to wake up at my goal weight and be a happier person. I thought the weight and the taunting was the problem, but it wasn't, the issue was the way I looked at myself; after years of being overweight, I just didn't feel like I was worth anything and I felt as if I still needed approval from people."
Happily, Jane has now learned to care less about what others think. "It's not that I don't care anymore - because everyone cares to a certain extent about what other people think of them - but I don't let it get to me anymore," she says. "I know that I am not going to be everyone's piece of cake, but what I have realised over time is that nobody is; you cannot please everyone.
"When you are overweight for so long you think weight loss is the answer to everything," Jane says.
"I was always living for the 'when' so 'when I lose a bit more weight I will do this or that,' but now I am at a stage where I don't put things off.
"I could have said 'I will lose three stone and I will apply for the Rose of Tralee next year,' but why? What is the difference? One very important thing I have learned is to try and accept who you are while you are losing weight because I did not, and I hit a low as a result of that."
Over time, Jane's mind has thankfully caught up with her body.
 55Wicklow Rose Jane Harrison lost 13 stone after gastric band surgery
55Wicklow Rose Jane Harrison lost 13 stone after gastric band surgery
"It took some big realisations and I definitely had to get in touch with myself a lot more. I got into spirituality and meditation and began to just work out what I want in life," Jane explains. "Now I know my triggers and when I've disconnected from the path I am on and I know how to get back on it."
Jane, who put off going to college after school because of her low self-esteem, is now enrolled on a college course in Communications and will represent Wicklow in the 2016 Rose of Tralee.
"I have decided to go for things I want now and not hold myself back and that is a huge part of why I entered the Rose of Tralee. I am definitely not at my dream weight and there are 100 things I would like to change about my figure, and I will still go to the gym and attempt to, but it doesn't consume me anymore like it did a few years ago," she says.
"When I go down to Tralee, it is going to be two weeks of food and drink and that doesn't freak me out at all, whereas two years ago the prospect of not having complete control over what I am eating would have really freaked me out," Jane admits. "I have a healthy approach to food and exercise now and I know what foods I can have and what I cannot have; I think when you just realise you want to be happy for yourself rather than others, that is when everything really clicks into place
Read more
Gastric band surgery for low BMI patients
He said that the long-term results from LABG had been achieved without any significant technological innovation of the device in the last 20 years
"Low BMI patients are a target population that as metabolic surgeons we need to take care of to prevent future morbid obese patients"

Thursday, September 15, 2016 - 09:21
Owen Haskins - Editor in chief, Bariatric News
At the recent European Obesity Summit in Gothenburg, Sweden, Apollo Endosurgery hosted a symposium, which included presentations on revisional surgery, long-term outcomes, low BMI patients, band complications and the banded bypass.

Luigi Angrisani
Patients who have a BMI30.0-34.0 (class 1) and who are suffering from a significant obesity-related health burden should be offered bariatric surgery, according to Luigi Angrisani, S Giovanni Bosco Hospital, Naples, Italy. In his presentation, ‘Low BMI patients: a target population to take care of to prevent future morbid obese patients, he cited a 2014 a Position Statement from the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) (Obesity Surgery. Bariatric Surgery in Class I Obesity – A Position Statement from the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) 2014), which states:“A clinical decision should be based on a more comprehensive evaluation of the patient’s current global health and on a more reliable prediction of future morbidity and mortality.”
Angrisani added that such a decision should take into account “more than just a patient’s BMI.”
He said that there an array of intragastric balloons (eg.Heliosphere Bag, Reshape Dual-balloon, Orbera, Spatz Adjustable Balloon System) and endoluminal procedures (eg. Apollo Overstitch, POSE and Endobarrier) that have shown weight loss in the short-term however, these devices/procedures have not yet proved long-term efficacy.
In comparison, the LAGB procedure has demonstrated long-term efficacy. Angrisani explained that in his own centre, between January 1996 and December 2015 they have carried out 107 bariatric procedures on obese patients with BMI≤35, and 32 patients received a LAGB. The ten year outcomes from these patients revealed on average patients lost 14kgs and the BMI was reduced from 33.78 to 29.6, with 40.2 average %EWL. Moreover, only three patients (9.3%) had their band removed.
He said that the long-term results from LABG had been achieved without any significant technological innovation of the device in the last 20 years (design, profile, material) or with little evolution of our knowledge in the last 15 years, such as the ability to calculate the ‘neo-pylorus’ diameter at time of band adjustment.
“Despite this lack of knowledge, the LAGB still remains an effective procedure and has demonstrated a high efficacy in low BMI and adolescents patients,” he concluded. “The LAGB has several advantages compared to more invasive procedures such as the absence of mortality and malnutrition, with no need for vitamin supplementation. Low BMI patients are a target population that as metabolic surgeons we need to take care of to prevent future morbid obese patients.”
Read more

New pre- and post-bariatric surgery diet resources launched
NDR-UK has launched two innovative new resources, developed by specialist dietetic colleagues at NHS Ayrshire and Arran, Scotland. The comprehensive, 80 page book is designed to support patients before and after gastric sleeve and gastric bypass surgery (not gastric band surgery - for information on this, please see resource 9014).
According to NDR-UK, the recipes have all been tried and tested and are easy to prepare and cook. They are high in protein and low in fat and calories. The ingredients are all easily sourced and the recipes are suitable for all the family. They are divided into breakfasts, soups, lunches, main meals and desserts. There are at least seven recipes in each section (for a week’s meals). All recipes are coded for different consistencies, whether able to be frozen and if vegetarian. The recipes have handy hints and are nutritionally analysed for a small, bariatric sized portion.
"In NHS Ayrshire and Arran we use the recipe books to support our pre-operative practical cooking session. The groups really enjoy these sessions, we find it encourages them to do more home cooking and to increase their awareness of portion sizes and optimal consistencies at different stages post-surgery. They are also really good fun!" said Pam Lindsay, Bariatric Dietitian, University Hospital Ayr, and co-author of 'Recipes for Life'
The book will soon be available to be purchased by the public, advising that is should be used in conjunction with the information given by a Specialist Bariatric Dietitian.
For further information, to view a sample or to order 'Recipies for Life' (9016), please click here
'Pre-operative 800Kcal Diet' Booklet (9015)
This 16 page booklet is for people preparing for bariatric surgery who need to follow a diet high in protein and low in calories (kcal), carbohydrate and fat for two weeks before their surgery. Three options of the 800kcal diet (often called the 'Liver Shrinkage Diet'): using normal consistency foods, soft/liquid meals or meal replacement drinks.
For further information, to view a sample or to order 'Pre-operative 800kcal diet' (9015), please click here
Read more

Gloheath covers your obesity surgery with Belgium Surgery Services and Dr Chris Debruyne.
Irish clients who are assured with Glohealth get their weightloss surgery with Belgium Surgery Services and Dr Chris Debruyne fully reimbursed. Due to our exellent reputation, low(est) rate of complications and Irish back-up network Glohealth and Laya Healtcare both reimburse weightloss surgery with Belgium Surgery Services.
GloHealth , Clearly different. Clearly Better.Clearly great cover.
For more information visit us at our consultation clinics in Dublin, Belfast or Killarney.
Read more

UK needs 50,000 bariatric procedures a year.
The NHS should significantly increase rates of bariatric surgery to 50,000 a year, closer to the European average, to bring major health benefits for patients and help reduce healthcare costs in the long term, according to a paper published in The BMJ. The paper states that between 2011-12 and 2014-15, the number of bariatric operations performed on the NHS fell by 31% - from 8,794 to 6,032, and less than 1% of those who could benefit get treatment. This is in stark contrast to provision in many European Union countries, as the UK currently ranks 13th out of 17 for EU countries and sixth in the G8 countries for rates of bariatric surgery. This is despite the UK having the second highest rate of obesity in Europe, and sixth internationally.
In the paper, ‘Why the NHS should do more bariatric surgery; how much should we do?’, the authors examine the clinical and cost effectiveness of bariatric surgery and examine the barriers to access.
“Increasing surgery rates to 50 000 a year, which is closer to the European average, could have major benefits for patient health and reduce direct healthcare expenditure within two years.”
With regards to the effectiveness of surgery the cite the Swedish Obese Subjects study (SOS), which reported weight loss being maintained for 20 years, with glycaemic control improved for at least ten years after surgery. In addition, surgical patients were more likely to go into glycaemic remission of diabetes and fewer patients progressed from pre-diabetes to diabetes. This study also noted that the average weight loss was 25-35% of body weight (usually at least 15 kg) after one year for patients who are severely obese and 15-25% after 20 years. This is compared with an average 7% weight loss achieved by patients undergoing an intensive lifestyle weight management programme or weight loss drugs.
Furthermore, data from the UK National Bariatric Surgical Registry showed that over 3,000 patients with diabetes who had bariatric surgery (between 2011 and 2013), some 65% had acceptable glycaemic control without medication after surgery.
The authors also state that bariatric surgery is cost effective compared with non-surgical treatments and a UK health technology assessment concluded that bariatric surgery for patients with BMI≥40 results in an incremental cost effectiveness ratio for of between £2000 and £4000 per quality adjusted life year (QALY) gained over 20 years. In addition, the diabetic and patients with BMI 30-39 the incremental cost effective ratio was £1367 per QALY gained. This is substantially below the £20,000 per QALY threshold for cost effectiveness used by the National Institute for Health and Care Excellence (NICE). They also argue that the cost of surgery is justified as a diabetic will need prescriptions, this costs alone is recouped within three years of surgery
Eligibility
According to guidance from the National Institute for Health and Care Excellence, surgery should be considered for the “severe obesity in whom all non-surgical measures have been tried without achieving or maintaining adequate weight loss” – this equates to some 1.6 million people in the UK who have a BMI>40.14.
In addition, there are another half a million people with diabetes and other obesity related disease with BMI≥35. An extra 60,000 people a year reach a BMI40 and the number of people with type 2 diabetes has also increased by 60% over the past decade (to 3.3 million or 5% of the adult population), with 9.5% of adults predicted to have the condition by 2030 (190,000 new patients each year). Despite this, bariatric surgery procedures have reduced dramatically in the UK, with no NHS operations in Northern Ireland and few in Wales and Scotland.
“Given the severity of the problem, it seems urgent to consider the potential barriers to surgery,” the authors note.
Read more

UK report: Early results show safety and efficacy of MGB
They reported mean weight loss of 45.6kg (range 16.1–112.7), percentage body weight loss of 33.2% (range 11.4–55.4), and percentage excess body weight loss of 71.8% (range 23.2–138.3)
The outcomes showed that there were no deaths, although there were two (3.2%) 30 day and five (4.0%) late (>30 day) complications.
The procedure was also seen as a success by patients who, when asked, 96% of patients said that they would elect to have the operation again, with 82.4% of patients reporting a vast improvement in their quality of life

Wednesday, March 16, 2016 - 12:07
Owen Haskins - Editor in chief, Bariatric News
The first early outcomes from UK from centre in the UK on mini gastric bypass (MGB), ‘Mini Gastric Bypass: first report of 125 consecutive cases from United Kingdom’, published in the journal Clinical Obesity, has reported that the results are ‘encouraging’ with acceptable weight loss, comorbidity resolution rates and complication profile. Although the study authors, from Sunderland Royal Hospital, Sunderland, UK, acknowledge that longer term follow-up data with greater patient numbers are required to confirm these outcomes, the study nevertheless “demonstrates early safety and efficacy of MGB in a carefully selected British obese population in a high-volume centre.”
The study authors note that there are several apparent advantages of the MGB compared with the RYGB, including the single anastomosis, shorter learning curve, fewer internal defects for herniation and ease of revision or reversal. However, due to concerns the procedure can cause symptomatic biliary reflux and the risk of gastric/oesophageal cancer has so far limited general acceptance of the procedure.
They subsequently designed a retrospective cohort study to report their experience with an initial cohort of 125 consecutive MGB patients starting in October 2012 (ended November 2014), with the first three procedures were performed with the help of an experienced MGB surgeon from abroad. As the majority of the patients at the study centre currently undergo a gastric bypass (either RYGB or MGB), all patients were considered to be included in the study, although the presence of Gastro-Oesophageal Reflux Disease (GORD) and/or hiatus hernia was a contraindication to MGB. However, patients with perceived technical difficulty for RYGB (super-obese, male, apple shaped body habitus), were offered MGB.
The procedure
The authors developed the following standardied technique for performing MGB: Closed pneumoperitoneum was established using optical insertion of 12mm port. This port was then used for camera insertion. Two further 12mm and one 5mm ports were used as working ports. A subxiphoid tract was created using 5mm port for insertion of Nathanson liver retractor. A long gastric pouch was created using Covidien TriStapler 45mm and 60mm Purple and Tan cartridges. Dissection was started at incisura and the first firing was carried out with stapler pointing towards the left iliac fossa.
A 36 French oro-gastric tube was used for pouch calibration in most cases (KM does not use it anymore). Omentum was not routinely divided. A loop of small bowel 200 cm from DJ flexure was then brought up to the gastric pouch in an ante colic, ante gastric fashion and anastomosed to it using Covidien Tristapler 45 mm Tan/Purple cartridge. Stapler entry site was then closed using 2/0 Vicryl in two layers. No attempt was made to close Petersen's defect and a leak test was performed using a dilute methylene blue solution. No drains were used.
From October 2012 to November 2014, 125 patients underwent MGB procedure a majority (68.8%) of these patients were female. The mean age of patients in this series was 45 (range 20–70) years, mean weight and BMI was 135.8 (range 85–244) kilograms and 48.1 (range 34.5–73.8), respectively. The mean operative time was 92.4 (range 45–150) minutes and the mean post-operative hospital stay was 2.2 (range 2–17) days (median 2.0 days). Fourteen patients had had previous bariatric intervention (13 balloon insertions, one sleeve gastrectomy).
Outcomes
The outcomes showed that there were no deaths, although there were two (3.2%) 30 day and five (4.0%) late (>30 day) complications.
The study authors noted 100% follow-up and the mean follow-up was 11.4 months. They reported mean weight loss of 45.6kg (range 16.1–112.7), percentage body weight loss of 33.2% (range 11.4–55.4), and percentage excess body weight loss of 71.8% (range 23.2–138.3). Figure 1 shows mean weight loss for the whole cohort at six, 12, 18 and 24 months with respective numbers available for follow-up at each time.

Figure 1: Weight loss after Mini Gastric Bypass. EWL, excess weight loss; TWL, total weight loss (Source: Clinical Obesity, John Wiley & Sons)
Comorbidities
At the start of the study, 33 (26.4%) patients has T2DM and all noticed improvement/resolution of their diabetes; 16 of the 33 (48.4%) patients were on Insulin preoperatively; 13 of them were able to stop their Insulin and the remaining three have seen reduction in their insulin doses. Eight patients have gone into remission. In addition, from 45 hypertensive patients, 13 (29%) have stopped anti-hypertensive medications and 22 (49%) have reduced their medications.
The procedure was also seen as a success by patients who, when asked, 96% of patients said that they would elect to have the operation again, with 82.4% of patients reporting a vast improvement in their quality of life.
“It is worth noting that RYGB still accounts for approximately 75% of the surgical procedures performed within our unit and MGB accounts for an approximate 15%,” they write. “Over the years, we also seem to be recommending MGB for the patients, who in the past were offered sleeve gastrectomy for perceived technical difficulty.”
They also comment on the link between MGB and the risk of gastric and/or oesophageal cancer, and state that they cannot find any evidence that the MGB procedure puts patients at a higher risk of cancers in the long term. Despite the lack of data, they do acknowledge that MGB will continue to be ignored by some critics who claim a lack of long term, in spite of a similar lack of long term data for gastric banding and sleeve gastrectomy.
“Other surgeons are well advised to make themselves aware of all the technical and controversial aspects of this procedure before embarking on it,” they write. “As we have seen it in our practice, even in the hands of experienced bariatric surgeons, this operation has a definite learning curve. The authors believe time is now ripe for a well-designed, multicentre, adequately powered randomised controlled trial comparing MGB with RYGB and sleeve gastrectomy.”
Read more
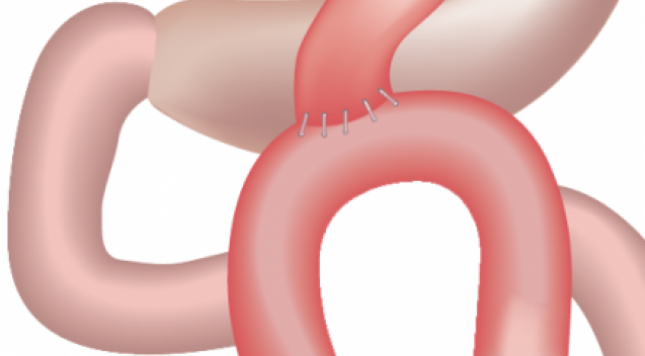
Omega-loop GB or MGB beats RYGB for weight loss
Omega-loop gastric bypass (OLGB) or Mini gastric bypass results in better weight loss (WL) compared to Roux-en-Y gastric bypass (RYGB), according to a retrospective study by researchers from the Medical University of Vienna, the Karl Landsteiner Institute for Obesity and Metabolic Diseases, Vienna and the Special Institute for Preventive Cardiology And Nutrition (SIPCAN), Salzburg, Austria. The study, ‘The Effect of Roux-en-Y vs. Omega-Loop Gastric Bypass on Liver, Metabolic Parameters, and Weight Loss’, published in Obesity Surgery, also reported that OLGB resulted in an increase of liver parameters in the first year after surgery, whist deteriorating after RYGB.
“The impact of these results on hepatic outcomes such as non-alcoholic steatohepatitis and fibrosis progression requires further studies. In both groups, improved insulin resistance and sensitivity were correlated with higher WL and lower liver fat percentage, respectively,” the authors write. “It remains unclear what induces the bimodal alteration in liver transaminases and cholestatic parameters during the early postoperative phase and also after 12 months.”
Due to the lack of data, the aim of the study was to compare the development of hepatic and metabolic markers as well as WL between the two surgical procedures during the first postoperative year. It is known that bariatric surgery can adversely affect the liver with several case reports of patients with early hepatic failure after surgery.
Therefore, the aim of this evaluation was to provide data on the development of hepatic and metabolic markers as well as on WL in morbidly obese patients undergoing either Roux-en-Y gastric bypass or omega-loop gastric bypass during the first 12 postoperative months to facilitate the design of studies in larger populations.
The authors stated that all procedures were performed by the same surgical team using a laparoscopic approach. RYGB consists of a longitudinal 30ml gastric pouch which is anastomosed end-to-side with the jejunal limb and a latero-lateral jejuno-jejunal anastomosis resulting in a biliopancreatic limb of approximately 80cm and an alimentary limb of approximately 150cm . Omega-loop gastric bypass is a simplified procedure that consists of a unique gastrojejunal anastomosis between a 30–40ml sleeve gastric pouch and a jejunal omega loop of 200cm.
The researchers retrospectively evaluated the respective parameters in non-diabetic morbidly obese patients who underwent either RYGB (n=25) or OLGB (n=25). The baseline charactistics were as follows: RYGB (n=25, female=92 %, 44.6 ± 10.3a, 125 ± 18 kg, BMI 45.6 ± 4.1) and OLGB (n=25, male=88 %, 43.8 ± 13.1a, 128 ± 24 kg, BMI 45.3 ± 5.3).
Outcomes
The results revealed that WL (mean ± SD) was 30 ± 9 vs. 38 ± 7 % (%BMI loss), which equals a percentage excess WL (%EWL) of 94 ± 36 vs. 127 ± 31 % or percentage excess BMI loss (%EBMIL) of 67 ± 22 vs. 88 ± 16 % in RYGB vs. OLGB after 12 months (OR = 1.19; 95 % CI = 1.11–1.27; p<0.001).
With regards to liver function, aspartate transaminase (AST), a significant group and time difference could be found, whereas alanine transaminase (ALT) dropped in Roux-en-Y gastric bypass, while rising in omega-loop gastric bypass with a significant group and time difference. Moreover, a positive correlation could be found between ALT, surgical method (r = 0.406, p = 0.006) and De Ritis ratio >1 (r = 0.451, p = 0.002) at 12 months. There was no correlation observed between WL, ALT, and AST was observed.
Initially, Omega-loop gastric bypass group showed a significant higher count in platelets, this difference disappeared at three months. Nevertheless, a difference between the groups, as well as a negative correlation with WL (r = −0.346, p=0.002) was found.
A significant group and time interaction also could be found for prothrombin time, as well as a significant increasing proportion of low prothrombin time in omega-loop gastric bypass at three months (RYGB vs. OLGB; operative date: 8 vs. 0 %, n.s.; three months: 5 vs. 8 %, p<0.05). A negative correlation between prothrombin time and WL was found in omega-loop gastric bypass (r = −0.543, p<0.001).
No differences appeared in the course of albumin, while protein diminished significantly over time and group. A negative correlation between protein and WL in both groups (r = −0.428, p<0.001), as well as for albumin and hsCRP (r = −0.611, p<0.01) in omega-loop gastric bypass was found at six months.
The authors also report that in the RYGB group, gamma-glutamyltransferase (GGT) significantly decreased by nearly half of the initial value, while it remained stable in OLGB and a significant group and time difference was found. Younger patients (<50 years) had a greater chance of lower GGT quartiles over time (p<0.001; adjusted for initial BMI). A negative correlation between GGT and WL could be seen in Roux-en-Y gastric bypass (p<0.001).
“The superiority of omega-loop gastric bypass over Roux-en-Y gastric bypass in terms of WL was demonstrated in previous studies, as well as in our study. We did not observe any influence of gender, age, or preoperative BMI on WL regardless of the procedure…Importantly, we could not detect a correlation between liver transaminases and WL,” they write.
NAFLD liver fat score showed a significant higher proportion of NAFLD in RYGB until six months (13 vs. 5 %, n.s). Liver fat percentage showed a similar development with a significant difference over time, and a strong correlation could be found between liver fat percentage and HOMA2-IR (p<0.001); QUICKI (p<0.001); AST (p<0.001); ALT (p<0.001); and TG (p<0.001) in both groups.
Glucose significantly decreased in both groups until one year. Insulin was significantly higher in RYGB post-operatively, although no group and time interaction could be found.
“Given the potential for worsening fibrosis following bariatric surgery, patients should be monitored closely and continue to undergo through hepatological workup, including non-invasive testing for fibrosis or, even liver biopsy. More research in this field, including histopathological data, is needed to define clinical relevance of these findings on hepatic outcome in terms of deterioration of non-alcoholic steatohepatitis and fibrosis and to characterise patients at risk,” the authors conclude. “In both groups, improved outcome in terms of insulin resistance and sensitivity could be found in correlation to higher WL and lower liver fat percentage, respectively.”
The article was edited from the original article, under the Creative Commons license. To access the article, please click here
Read more

Excellent New Habits after Bariatric Surgery
After Bariatric Surgery, you will begin to look around your kitchen with new eyes, and as you make your weekly grocery list, there will be so many things you will no longer want to buy. Don’t worry – it will get easier as the days go by and soon, you will have some healthy new habits to add years to your life, but how can you speed those new habits along, helping make sure you see and enjoy the results of weight loss surgery long term?
New Habits after Bariatric Surgery
Here are some quick kitchen tips for those of you who want to make your kitchen weight loss friendly after Bariatric surgery and help speed those new habits along. Don’t be discouraged if you make a mistake. It took a lifetime to learn all of these unhealthy eating habits, so don’t be too hard on yourself! Every day is a clean slate and a fresh start on your road toward a healthy weight and proper nutritional habits.
Buy Bottled Water after Weight Loss Surgery
While you may have wonderfully tasting well or tap water that runs into your glass for free, you are probably willing to admit that you aren’t drinking the required number of glasses per day. After Bariatric surgery, it is highly recommended that you purchase bottled water and store it in the refrigerator or another cool location.
You will find that using purchasing bottled water will motivate you, and help you keep track of your daily water intake goals. You may be able to get your family involved with a little competitive cross referencing with the other water drinkers in your home. Do not mistake distilled water for healthy bottled water, which is not nearly as healthy and beneficial for your body.
Boiled Eggs after Bariatric Surgery
After weight loss surgery, you will have to follow a very specific diet until your stomach has healed and you are no longer on a liquid, puree or soft food regimen. Once you have been approved for regular food, you will be looking for high protein recipes that meet the needs of your new lifestyle. Breakfast can be especially difficult since you no longer need to eat toast, biscuits, sugary sweet cereal or greasy pork bacon and sausage.
However, what you can have are protein rich eggs. Most nutritionists will tell you that eating at least one hard boiled egg each morning for breakfast will increase your energy levels by 70 percent. This is because protein is fuel for the body and eggs are a fast, affordable and easy source. Make a new habit of keep a small container of hard boiled eggs in the refrigerator. You will find that this is a fast and convenient breakfast that you will learn to appreciate. Sprinkle some paprika on them for a bit of flavor if you do not like them plain, as this spice is a great source of vitamin E.
Individual Sweeteners Packets for Bariatric Patients
After Bariatric surgery, you will no longer be able to enjoy sugary sweet drinks and treats. You can, however, have artificial sugar. If one of your old habits included drinking sweet iced tea, Kool-aid or coffee with sugar, you should consider purchasing artificial sweeteners in individual packets. While drinks won’t taste nearly as sweet, you will find that over time, you can train your taste buds to enjoy less.
Another great benefit of pre-measured packets is you can see exactly how many calories you are drinking and how much progress you’ve made. Also, these pre-measured packets can be carried in a purse or pocket, making it easy to maintain your new habit wherever you go.
Zipper Seal Bags for Weight Loss Surgery Patients
After you have undergone Bariatric surgery, portion control becomes an important issue and plastic zipper seal bags can be a huge help in the storing and cooking process. While you can save significantly by buying in bulk, you should re-package all meat and food items into zipper seal bags that contain only enough for the number and size of the meals you will need.
Not only will you avoid over-eating and later raiding the fridge for leftovers, you will also find that packages used to make one dinner meal might stretch much further now. It won’t take long before you are hooked on buying and using these household helpers.
What are some other items to help build new habits after Bariatric surgery?
Read more

UK report: Early results show safety and efficacy of MGB
The first early outcomes from UK from centre in the UK on mini gastric bypass (MGB), ‘Mini Gastric Bypass: first report of 125 consecutive cases from United Kingdom’, published in the journal Clinical Obesity, has reported that the results are ‘encouraging’ with acceptable weight loss, comorbidity resolution rates and complication profile. Although the study authors, from Sunderland Royal Hospital, Sunderland, UK, acknowledge that longer term follow-up data with greater patient numbers are required to confirm these outcomes, the study nevertheless “demonstrates early safety and efficacy of MGB in a carefully selected British obese population in a high-volume centre.”
The study authors note that there are several apparent advantages of the MGB compared with the RYGB, including the single anastomosis, shorter learning curve, fewer internal defects for herniation and ease of revision or reversal. However, due to concerns the procedure can cause symptomatic biliary reflux and the risk of gastric/oesophageal cancer has so far limited general acceptance of the procedure.
They subsequently designed a retrospective cohort study to report their experience with an initial cohort of 125 consecutive MGB patients starting in October 2012 (ended November 2014), with the first three procedures were performed with the help of an experienced MGB surgeon from abroad. As the majority of the patients at the study centre currently undergo a gastric bypass (either RYGB or MGB), all patients were considered to be included in the study, although the presence of Gastro-Oesophageal Reflux Disease (GORD) and/or hiatus hernia was a contraindication to MGB. However, patients with perceived technical difficulty for RYGB (super-obese, male, apple shaped body habitus), were offered MGB.
The procedure
The authors developed the following standardied technique for performing MGB: Closed pneumoperitoneum was established using optical insertion of 12mm port. This port was then used for camera insertion. Two further 12mm and one 5mm ports were used as working ports. A subxiphoid tract was created using 5mm port for insertion of Nathanson liver retractor. A long gastric pouch was created using Covidien TriStapler 45mm and 60mm Purple and Tan cartridges. Dissection was started at incisura and the first firing was carried out with stapler pointing towards the left iliac fossa.
A 36 French oro-gastric tube was used for pouch calibration in most cases (KM does not use it anymore). Omentum was not routinely divided. A loop of small bowel 200 cm from DJ flexure was then brought up to the gastric pouch in an ante colic, ante gastric fashion and anastomosed to it using Covidien Tristapler 45 mm Tan/Purple cartridge. Stapler entry site was then closed using 2/0 Vicryl in two layers. No attempt was made to close Petersen's defect and a leak test was performed using a dilute methylene blue solution. No drains were used.
From October 2012 to November 2014, 125 patients underwent MGB procedure a majority (68.8%) of these patients were female. The mean age of patients in this series was 45 (range 20–70) years, mean weight and BMI was 135.8 (range 85–244) kilograms and 48.1 (range 34.5–73.8), respectively. The mean operative time was 92.4 (range 45–150) minutes and the mean post-operative hospital stay was 2.2 (range 2–17) days (median 2.0 days). Fourteen patients had had previous bariatric intervention (13 balloon insertions, one sleeve gastrectomy).
Outcomes
The outcomes showed that there were no deaths, although there were two (3.2%) 30 day and five (4.0%) late (>30 day) complications.
The study authors noted 100% follow-up and the mean follow-up was 11.4 months. They reported mean weight loss of 45.6kg (range 16.1–112.7), percentage body weight loss of 33.2% (range 11.4–55.4), and percentage excess body weight loss of 71.8% (range 23.2–138.3). Figure 1 shows mean weight loss for the whole cohort at six, 12, 18 and 24 months with respective numbers available for follow-up at each time.

Figure 1: Weight loss after Mini Gastric Bypass. EWL, excess weight loss; TWL, total weight loss (Source: Clinical Obesity, John Wiley & Sons)
Comorbidities
At the start of the study, 33 (26.4%) patients has T2DM and all noticed improvement/resolution of their diabetes; 16 of the 33 (48.4%) patients were on Insulin preoperatively; 13 of them were able to stop their Insulin and the remaining three have seen reduction in their insulin doses. Eight patients have gone into remission. In addition, from 45 hypertensive patients, 13 (29%) have stopped anti-hypertensive medications and 22 (49%) have reduced their medications.
The procedure was also seen as a success by patients who, when asked, 96% of patients said that they would elect to have the operation again, with 82.4% of patients reporting a vast improvement in their quality of life.
“It is worth noting that RYGB still accounts for approximately 75% of the surgical procedures performed within our unit and MGB accounts for an approximate 15%,” they write. “Over the years, we also seem to be recommending MGB for the patients, who in the past were offered sleeve gastrectomy for perceived technical difficulty.”
They also comment on the link between MGB and the risk of gastric and/or oesophageal cancer, and state that they cannot find any evidence that the MGB procedure puts patients at a higher risk of cancers in the long term. Despite the lack of data, they do acknowledge that MGB will continue to be ignored by some critics who claim a lack of long term, in spite of a similar lack of long term data for gastric banding and sleeve gastrectomy.
“Other surgeons are well advised to make themselves aware of all the technical and controversial aspects of this procedure before embarking on it,” they write. “As we have seen it in our practice, even in the hands of experienced bariatric surgeons, this operation has a definite learning curve. The authors believe time is now ripe for a well-designed, multicentre, adequately powered randomised controlled trial comparing MGB with RYGB and sleeve gastrectomy.”
Read more

Thousands of Irish patients need weightloss Surgery
Thousands of Irish patients could have their life expectancy significantly increased and chronic diseases reversed following obesity surgery, new research suggests.
In a paper to be presented in early September researchers at Galway university hospital and the Galway Clinic followed 118 morbidly obese patients for two years after they underwent gastric bypass surgery. The sustained average excess body weight loss experienced by patients in the study was 55 per cent after two years.
Of patients with pre-existing high blood pressure, more than 80 per cent required less medication after surgery. Two-thirds of those with pre-existing diabetes were able to discontinue medication after the procedure. Some four in 10 with high blood pressure no longer required anti-hypertensive medication after the laparoscopic sleeve gastrectomy (LSG) operation.
Stomach removed
LSG is a weight-loss bariatric procedure in which a large portion of the stomach is removed, reducing it to a quarter of its original size. The restricted size of the stomach leads to a reduced intake of food and a feeling of being full earlier in a meal. The benefits of LSG are not just due to reduced gastric capacity but also because it modifies the release of gastrointestinal hormones.
Most of the patients in the Galway study, which will be presented at the Freyer international surgical symposium at NUIG on September 5th, had a body mass index (BMI) of 40 or more. All participated in a rigorous long-term weight loss programme before referral for consideration for bariatric surgery. There were no deaths in the study group.
Prof Oliver McAnena, consultant gastrointestinal surgeon at Galway university hospital (GUH) and the Galway Clinic, who operated on the patients in the study said, “Studies have shown the life expectancy of people with severe obesity is severely compromised if they are not offered the option of bariatric surgery. It is a cost-effective intervention but is a serious operation that requires careful patient selection.”
Thousands affected
Co-author Dr Francis Finucane, consultant endocrinologist at GUH, said that 1-2 per cent of Irish people severely affected by obesity could benefit from bariatric surgery. “However only a proportion of the thousands of Irish people affected will be suitable for bariatric surgery or will seek it,” he said.
While acknowledging plans for the State to fund 400 bariatric operations annually by 2018, Dr Finucane said, “There is an element of discrimination of obese patients that limits the application of surgery. If this was cancer or heart disease, and not severe obesity . . . these surgical interventions would be used more widely.”
The latest figures show that 23 per cent of Irish men and 22.5 per cent of Irish women are obese ie their BMI is over 30. Many people who lose weight regain it over time.
Weight loss surgery is now recognised as an effective and appropriate treatment for patients with a BMI of 40, or a BMI of 35 with related illnesses such as diabetes and hypertension
Read more

NHS’s approach to obesity is “failing patients”
A case study entitled Confronting Obesity in the UK: The need for greater coherence has been published today by the Economist Intelligence Unit (EIU), with experts calling for a coherent strategy to tackle obesity1. The study explores the UK’s approach to obesity management and interviews experts, highlighting that commitment to a multi-stranded programme and cultural change is needed to enable obesity services in the UK to live up to their potential.
According to Dr Matthew Capehorn, clinical manager of the Rotherham Institute for Obesity (RIO) in South Yorkshire, who was interviewed for the case study, £5bn is spent on prevention strategies, leaving just £300m for treatment. The case study reveals that the continued structural reform of the UK healthcare system has led to confusion over accountability, creating huge differences in access to treatment. According to Capehorn, only 60% of obesity services across the UK have access to higher levels of treatment, but the level of access varies significantly.
“The UK has excellent evidence based guidelines from National Institute of Health and Care Excellence detailing strategies for the prevention and management of obesity in children and adults. We now need to ensure that these are implemented” said Professor Rachel Batterham, Head of the UCLH Bariatric Centre for Weight Management and Metabolic Surgery and the UCL Centre for Obesity Research. “We know that for some patients, especially those with type 2 diabetes, that bariatric surgery leads to unrivalled health benefits and cost-saving for the NHS. Unfortunately, less than 1% of the patients who could benefit from this surgery currently receive surgery. This represents a major missed opportunity in terms of improving health and economic savings”*.
Obesity is a rising concern in the UK with 62% of the population now overweight or obese2. Yet, according to the case study, the shortage of obesity services is negatively impacting patients; as people with severe obesity are forced to wait longer to be assessed, have their associated medical problems treated and receive weight-loss advice.
Obesity is a major public health concern across Europe and the UK is no exception. Due to its association with serious chronic diseases such as type 2 diabetes, cardiovascular disease and some cancers3, obesity places a huge burden on both the UK’s health and economy. The study highlights that the one quarter of the population that is obese cost the NHS £6bn–8bn alone in 20154. By 2025 the NHS cost of all weight related disease is predicted to reach £21.5 billion per year4,over 20% of the current NHS budget.
The study, which was commissioned by the Johnson and Johnson subsidiary, Ethicon, follows the release of an EIU report entitled, Confronting Obesity in Europe: Taking action to change the default setting. The report highlights the need for European policymakers to address the impending health crisis and stresses that national approaches to obesity need to take into account two distinct populations: those of a healthy weight and those who are already severely obese5.
“The study suggests that a more holistic and cost effective strategy is needed to tackle obesity, and we believe that bariatric surgery could play an important role here” said Silvia De Dominicis, Vice President of Ethicon EMEA. “At Ethicon, we pride ourselves on value-based healthcare and we’re committed to supporting patients in the UK. We hope that this case study helps to open up an urgently needed discussion with policymakers and shape the future of the obesity strategies. It’s time to act.”
Read more

Gastric band and nutritional deficiencies
A new book has been launch that contains useful and practical advice, questionnaires, hints and tips to maximise weight-loss and support overall long-term health, following laparoscopic gastric band surgery. Co-authored by registered nutritional therapists, Nicola M Pearson and Claudia Williamson, this practical handbook has been specifically written for gastric band patients. The book is fully referenced so that nutrition and bariatric professionals can also use it with confidence, knowing that it is evidence based. Each chapter is clearly written, based on science but highly readable, and is summarised so the band patient has a clear vision of what is relevant to them, their weight and their health.
Read more

Bariatric surgery can improve fertility
A report by the Royal College of Obstetricians and Gynaecologists (RCOG) in the UK has found that bariatric surgery can improve fertility. The report entitled, ‘The Role of Bariatric Surgery in Improving Reproductive Health’, examined the safety and effectiveness of bariatric or weight loss surgery as a way of improving female fertility and reproductive health in obese women, and concluded that bariatric surgery improves a woman’s fertility and reduce pregnancy complications. This new report is the second report from the RCOG on the role of bariatric surgery on female fertility, the first edition was called The Role of Bariatric Surgery in the Management of Female Fertility (2010).
Roger Ackroyd
"We welcome the RCOG report which has valuable insights and we agree entirely that bariatric surgery is indeed often beneficial to overweight women wishing to become pregnant,” said Mr Roger Ackroyd, President of the British Obesity and Metabolic Surgery Society. “Not only does it increase fertility in women who are often less fertile due to their weight and/or polycystic ovaries, but it can decrease problems and complications of pregnancy and in the newborn. NICE Guidelines now recommend surgery down to a BMI30 in patients with Type 2 diabetes which may include many women of child-bearing age."
It is known that obesity has a negative impact on natural conception, miscarriage, pregnancy and the long term health of the mother and child due to an increased rate of birth defects, pregnancy complications and the possibility of disease later in life. Furthermore, obesity is a common problem among women of reproductive age with 26 percent of women in the UK reported to have a BMI>30. In addition, women are three times as likely to be admitted to hospital with a primary diagnosis of obesity as men and female patients outnumber male patients seeking bariatric surgery by a ratio of around 3:12 - approximately 70% of these women are of childbearing age. Indeed, one study found that 25% (29/115) of women presenting for bariatric surgery suffered from infertility.
However, research has suggested that bariatric surgery does improve female fertility, including an improvement in symptoms of polycystic ovary syndrome (PCOS) which influences fertility, the release of eggs, hormonal changes, sexual activity and libido. In addition, surgery can also reduce pregnancy complications when compared to untreated obese women or previous pregnancies in the same women, including a reduced risk of miscarriage, gestational diabetes, hypertension, macrosomia (large baby) and congenital abnormalities.
This latest paper reviews the most recent evidence on the safety and efficacy of bariatric surgery as an intervention to improve female fertility and reproductive outcomes in obese women.
Read more
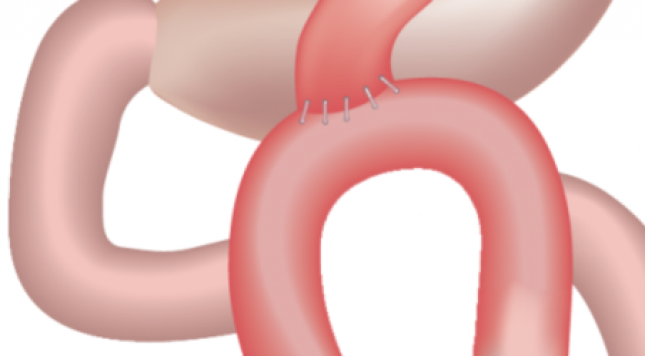
Mini Gastric Bypass ( MGB ) in resolution of Diabetes
Bariatric Surgeon, Gurvinder S Jammu and nutritionist/dietitian Rajni Sharma, MSc, audited 1,107 cases, comparing SG, RYGB and MGB, at the Jammu Hospital, Jalandhar, state of Punjab in Northwest India. Their seven-year data (Jan 2007 to Mar 2014) was collected prospectively and reviewed retrospectively, with a database of 473 MGBs, 339 LSGs, and 295 RYGBs. The study, 'A 7-Year Clinical Audit of 1107 Cases Comparing Sleeve Gastrectomy, Roux-En-Y Gastric Bypass, and Mini-Gastric Bypass, to Determine an Effective and Safe Bariatric and Metabolic Procedure', was reported in Obesity Surgery (online first).
India is known for prevalence of undernutrition, but a significant obese population co-exists. Punjab is one of the most obese states in India with incidence 33.8%. Impaired glucose tolerance with metabolic syndrome has frequent onset in South-east Asians at BMI >22.
Patients were assessed for nutritional status, medical fitness and psychological well-being by the bariatric surgeon, physician, anesthetist, and bariatric counselor. Patients were presented with three options in detail – LSG, RYGB and MGB after one-on-one consultations with surgeon and medical team. Written informed consent was obtained from all patients.
MGB used the Rutledge technique with first stapler firing perpendicular to lesser curvature distal to crow’s foot, followed by vertical gastric division proximally to the left of the angle of His (which was not dissected). Next, jejunum was measured to 200cm distal to Treitz’ ligament, where a wide antecolic gastrojejunostomy was performed (leading to low intraluminal pressure).
LSG was started by dissecting across antrum 3-5 cm proximal to pylorus.
Laparoscopic RYGB created a 30-50 ml gastric pouch to the lesser curvature, with the jejunum transected 50 cm distal to Treitz’ ligament, with the proximal divided end of jejunum anastomosed 75 cm distally, where a side-to-side entero-enteral anastomosis was done.
For %EWL and resolution of co-morbidities, only patients with mean follow-up of 53.5 months (20-87 months) made up the patient material. Follow-up was by monthly visits, phone calls and email. Data included outcomes at 30 days, three months, six months, one year, and yearly thereafter. All patients signed a declaration that they will stay in contact throughout life, either in person/phone/email.
Follow-up was first year 94.7%, second year 90.8%, third year 81.4%, fourth 75.1%, fifth 72.2%, sixth 68.9%, and seventh year 52.7%. The three operative groups were demographically comparable in age, sex and weight.
Mean operating time was 60.0mins for LSG, 160.5mins for RYGB and 57.5mins for MSG. Mortality was 2.1% in LSG, 0.3% in RYGB, and zero in MGB. Leaks were highest in LSG (1.5%), followed by RYGB (0.3%) and zero in MGB. One patient after LSG had persistent vomiting which progressed to Wernicke’s encephalopathy. Bile reflux was seen transiently in 0.4% after MGB. GERD occurred in 9.4% after LSG, 1.7% after RYGB, and 0.6% after MGB.
One patient after RYGB had marginal ulceration (a smoker who improved with conservative methods). Three patients after MGB had marginal ulcer, and all responded to conservative management – PPI, yoghurt and cessation of cigarettes, NSAIDs and alcohol. One patient after RYGB had persistent vomiting one year post-op, which responded to endoscopic dilatation of a stenosis. There was no internal hernia after LSG and MGB but it occurred in 2.0% after RYGB.
Resolution of type 2 diabetes, dyslipidemia, and hypertension was maximal in MGB. In resolution of diabetes, MGB showed specular results: 94.4% stopped diabetic medications a few weeks after MGB, 76.2% after RYGB and 59.4% after LSG.
Read more
Obesity solutions: Mini Gastric Bypass/MGB is safe and effective
Laparoscopic mini gastric bypass (LMGB) is at least not inferior to laparoscopic gastric bypass (LRYGB), laparoscopic adjustable gastric banding (LAGB) and laparoscopic sleeve gastrectomy (LSG) in terms of weight loss and type 2 diabetes (T2DM) remission and has few complications. These are the conclusions from a met-analysis by researchers from Fudan University Pudong Medical Center, Shanghai, China, who state that future clinical trials are still needed to demonstrate its utility and establish the guidelines for LMGB.
The paper, ‘Efficacy of Laparoscopic Mini Gastric Bypass for Obesity and Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis,’ published in the journal Gastroenterology Research and Practice, is a systematic review and meta-analysis that evaluates and compares the efficacy, advantages and complications of LMGB with those of LAGB, LSG, and LRYGB, and reports the evidence to support the use of LMGB in treating obesity and T2DM.
The researchers conducted the literature search that identified 31 articles: 16 non-controlled single-arm case studies reported the surgical outcomes of LMGB, eight studies compared LMGB with LAGB, six studies compared LMGB with LSG and five studies compared LMGB with LRYGB; they were included in the meta-analyses, respectively. Overall, 16 studies reported the outcomes of LMGB for obese patients with participants ranging from 10 to 2,410. Female patients were predominant and mean BMI>35 in most studies. The percentages of patients with T2DM varied from 0 to 100%.
Read more

Obesity increases breast cancer risk in postmenopausal women
An analysis of extended follow-up data from the Women's Health Initiative clinical trials suggests that postmenopausal women who were overweight and obese had an increased risk of invasive breast cancer compared to women of normal weight, according to an article, ‘Overweight, Obesity, and Postmenopausal Invasive Breast Cancer Risk - A Secondary Analysis of the Women’s Health Initiative Randomized Clinical Trials’, published online by JAMA Oncology.
Dr Marian L Neuhouser of the Fred Hutchison Cancer Research Center in Seattle, and co-authors examined the association between being overweight and obese with the risk of postmenopausal invasive breast cancer. The Women's Health Initiative (WHI) protocol measured height and weight, baseline and annual or biennial mammograms, and breast cancer in 67,142 postmenopausal women enrolled from 1993 to 1998 with a median of 13 years of follow-up. There were 3,388 invasive breast cancers.
Analysis by the authors found:
- Women who were overweight (body mass index [BM] 25 to < 30); obese, grade 1 (BMI 30 to < 35); and obese, grade 2 plus 3 (BMI greater than 35) had an increased risk of invasive breast cancer compared to women of normal weight (BMI < 25)
- The risk was greatest for women with a BMI greater than 35; those women had a 58 percent increased risk of invasive breast cancer compared with women of normal weight (BMI < 25)
- A BMI of 35 or higher was associated with increased risk of estrogen and progesterone receptor-positive breast cancer but not estrogen receptor-negative cancers
- Obesity was associated with markers of poor prognosis; women with a BMI greater than 35 were more likely to have large tumors, evidence of lymph node involvement and poorly differentiated tumors
- Women with a baseline BMI of less than 25 who gained more than 5 percent of body weight during the follow-up period had an increased risk of breast cancer
- Among women who were already overweight or obese there was no association of weight change (gain or loss) with breast cancer during follow-up
- There was no effect on the BMI-breast cancer relationship from postmenopausal hormone therapy (HT)
'Obesity is associated with a dose-response increased postmenopausal breast cancer risk, particularly for oestrogen receptor- and progesterone receptor-positive disease, but risk does not vary by HT use or race/ethnicity. These clinically meaningful findings support the need for clinical trials evaluating the role of obesity prevention and treatment on breast cancer risk,' the article concludes.
In a related commentary, ‘Obesity and Breast Cancer - Narrowing the Focus’, Dr Clifford Hudis of Memorial Sloan Kettering Cancer Center, New York, and Dr Andrew Dannenberg of the Weill Cornell Medical College, New York, write: '…In addition to identifying an increased risk for women who are overweight or obese, their data suggest a dose-response relationship with higher BMI categories associated with greater relative risk. The collection of WHI clinical trials includes some in which oestrogen supplementation (alone or with progesterone) was tested, but they note no significant modification of risk with the use of hormone replacement therapy. Finally, they did not detect a change in risk for hormone receptor–negative breast cancers. Considering earlier observations suggesting a protective effect for obesity among premenopausal women, Neuhouser et al help refine our understanding of the risk of overweight and obesity; it is a particular concern for the most common form of breast cancer, hormone receptor–positive postmenopausal disease…we need a better understanding of the interrelated roles of not only calorie-restricted diets but also specific dietary composition(s) and various exercise programs deployed in specific patient groups…Overweight and obesity are a growing global challenge and the increased burden of malignant disease, to which it contributes, is another one. Their report helps focus our thinking and motivates us to pursue a deeper understanding of why overweight and obesity are a problem so that we can plan more effective and thoughtful responses.”
Read more

New weightloss and cosmetic clinic in Bristol and Edinburgh 2015
Looking for weightloss or cosmetic surgery abroad ? Belgium Surgery Services is your partner to guide you from start to finish. All patients are welcome at our new clinics for a Free of Charge initianal consultation.
Further we will continuous our gastric band afteracre servicesat our new clinics .Gastric band fills for all patients available for 90£ only.
Find the new addresses and dates on our website: www.belgiumsurgeryservices.co
Read more

Mini gastric bypass or single-anastomosis bypass – an attractive alternative?
According to a paper published in the Scandinavian Journal of Surgery, the single-anastomosis gastric bypass “may be an attractive alternative metabolic operation”. Also known as the one-anastomosis gastric bypass or mini gastric bypass, the procedure can result in a shorter operative time, fewer short- and long-term complications, improved and sustained excess weight loss and is more effective in terms of resolutions of comorbidities compared to standard RYGB, the paper states.
Introduced by Dr Robert Rutledge in 2001, the single-anastomosis bypass has increased in popularity due to its simplicity and apparent safety and effectiveness. The benefits include:
- fewer sites for leakage and internal hernia
- easier and faster to learn and perform
- easier to reverse and revise
Read more
Obese women 40% more likely of getting weight-related cancer
Obese women have around a 40 per cent greater risk of developing a weight-related cancer in their lifetime than women of a healthy weight, according to new figures released by Cancer Research UK. Obesity increases a woman’s risk of developing at least seven types of cancer including bowel, post-menopausal breast, gallbladder, womb, kidney, pancreatic and oesophageal cancer. The new statistics find that obese women have around a one in four risk of developing a cancer linked to weight in their lifetime.
“Losing weight isn’t easy, but you don’t have to join a gym and run miles every day or give up your favourite food forever. Just making small changes that you can maintain in the long term can have a real impact,” said Dr Julie Sharp, head of health information at Cancer Research UK. “To get started try getting off the bus a stop earlier and cutting down on fatty and sugary foods. Losing weight takes time so gradually build on these to achieve a healthier lifestyle that you can maintain. And find out about local services, which can provide help and support to make lifestyle changes over the long term.
In a group of 1,000 obese women, 274 will be diagnosed with a bodyweight-linked cancer in their lifetime, compared to 194 women diagnosed in a group of 1,000 healthy weight women. Approximately a quarter of UK women are obese which puts them at a greater risk of cancer. There are different ways that obesity could increase the risk of cancer, and one possibility is that it is linked to a fat cell’s production of hormones, especially oestrogen. This hormone is thought to fuel the development of cancer.
“We know that our cancer risk depends on a combination of our genes, our environment and other aspects of our lives, many of which we can control – helping people understand how they can reduce their risk of developing cancer in the first place remains crucial in tackling the disease,” she added. “Lifestyle changes – like not smoking, keeping a healthy weight, eating a healthy diet and cutting back on alcohol – are the big opportunities for us all to personally reduce our cancer risk. Making these changes is not a guarantee against cancer, but it stacks the odds in our favour.”
The following* shows the increased lifetime cancer risk for obese women by cancer type, compared with women of a healthy weight:
- Breast cancer (postmenopausal) 25%
- Pancreas cancer 31%
- Bowel cancer 32%
- Kidney cancer 78%
- Gallbladder cancer 100%
- Uterus (endometrium) cancer 131%
- Esophageal cancer 133%
Read more

Mini gastric Bypass, a safe and effective weightloss procedure.
A team of French researchers have reported that the single anastomosis or mini-gastric bypass is safe and effective in the long-term with outcomes comparable to those of RYGB. Reporting their findings in three separate papers, they added that the procedure is technically simple and is an option that should be considered by all bariatric surgeons.
In the first paper featured in the journal Surgery of Obesity and its Related Diseases, the investigators from the Hôpital Européen Georges Pompidou, Paris, France, examined the five-year results of 175 patients who had undergone a laparoscopic mini-gastric bypass (LMGB) between October 2006 and October 2008. Complete date was available in 126 of 175 patients (72%).
They assessed the mortality, morbidity, weight loss, co-morbidities, and quality of life - the latter was analysed using the Gastrointestinal Quality of Life Index (GIQLI) and was compared with a retrospectively case matched preoperative control group.
They reported a 0% mortality rate with 13 patients (10.3%) developing major complications including; marginal ulcers (4%), incapacitating biliary reflux (1.6%), gastric pouch dilation (3.2%) and inadequate weight loss with severe malnutrition (1.6%).
At five-years, the mean BMI was 31±6 and mean %EBMIL was 71.5%±26.5%. Postoperative GIQLI score of the treatment group was significantly higher than preoperative score of the control group (110.3±17.4 versus 92.5±15.9, p<.001). Social, psychological, and physical functions were increased significantly. No significant differences were found in gastro-oesophageal reflux or diarrhoea symptoms between the two groups. Long-term follow-up showed an improvement in all co-morbidities.
They concluded that at five-years, LMGB was safe, effective, and provided interesting quality of life results.
In the second paper, published in .Obesity Surgery, they reported that single anastomosis gastric bypass is an effective procedure for morbid obesity with comparable outcomes to RYGB.
Data was collected on 1,000 consecutive patients, with a mean follow-up period of 31 months. They noted a mortality rate of 0.2 % and an overall morbidity rate of 5.5 %. Thirty four patients required reoperations: six leaks, five obstructions, five incisional hernias, seven biliary refluxes, two perforated ulcers, two bleeds, two abscesses, and one anastomotic stricture, with four patients required a re-operation for weight regain.
At five-years, percent excess body mass index loss was 71.6±27 %. One hundred patients with type-2 diabetes, with a mean preoperative HbA1C of 7.7 ± 1.9 %, were followed for more than two years and the total resolution rate was 85.7 %.
They concluded that the study results not only confirm that MGB is an effective procedure but its appears to be safer than RYGB with a lower morbidity.
The third paper, published in Surgical Endoscopy, reported the outcomes from MGB in terms of its impact on type 2 diabetes.
Between December 2006 and September 2012, 804 laparoscopic MGB were performed, with 100 (12.4 %) patients having a glycated haemoglobin (HbA1c) level of <6 % without concomitant treatment.
Prior to the procedure seven patients (9%) had received no oral hypoglycaemic treatment, 30 (37%) had received monotherapy, 26 (32%) bitherapy, six (7%) tritherapy and 12 (15%) patients had used insulin. Over a mean follow-up of 26 months (range 1-75), mean weight decreased to 94±23 kg and mean BMI 35.
They report that 71 (88%) patients had complete remission of type 2 diabetes and the other ten (12 %) had reduced their treatment. Seven patients (58%) who were initially treated with insulin, no longer required insulin. The mean time to remission of diabetes for patients receiving one or more oral therapies versus insulin was 6.9 versus 17.9 months.
In conclusion the authors said the procedure is an effective treatment for obesity in terms of weight loss and remission of type 2 diabetes.
Read more

New weightloss and plastic surgery clinics at Bristol
Form April onwards Belgiums Surgery Services will open a new clinic in Bristol .
The clinic is availble for all patients that need gastric band aftercare ,weightloss support or inquire for obesity or plastic surgery.
Our brand new office based in an ultra modern facility will reflect the quality and proffesionalisme of our services.
The address and dates of our New clinic in Bristol will be soon displayed on our website:
Clifton physiotherapy clinic
118 Hampton Road
Redland
Bristol
BS6 6JD
Read more

Gastric band aftercare Manchester : address change Calderbank Medical Chambers
Dear All,
From March onwards Calderbank Medical Chambers will be based at 599 Wilmslow Road, Didsbury
Manchester M20 3 QD.
We hope to welcome you soon at our new offices.
Read more
Britain's obesity death rate: Belgium Surgery Solution = Gastric band 3200£, Sleeve 4850£, Gastric Bypass 5600£
More people are dying in Britain due to being overweight or obese than anywhere else in Europe, a study revealed yesterday.
Around one in every 11 deaths in the UK is now linked to carrying excess fat - 50 per cent more than the rate in France.
Experts also warned that the number of fatalities due to obesity may soon, for the first time, exceed those caused by smoking.
Being overweight or obese leaves people at high risk of heart disease, diabetes, high blood pressure and osteoarthritis. It also makes them much more likely to develop several types of cancer.
The growing health disaster is being blamed on the rise of aggressively marketed, fatladen fast food and couchpotato lifestyles.
Around half of British adults are overweight, and 17 per cent of men and 21 per cent of women are obese.
The difference between being overweight and obese lies in a person's Body Mass Index, which is calculated from weight and height. An adult with a BMI of more than 25 is classed as overweight and one with a BMI of more than 30 is obese.
Britain is the 'fat capital' of Europe, according to researchers from the University of Madrid's School of Medicine whose study is published in the European Journal of Clinical Nutrition.
The lowest death rate from being obese and overweight was in France, but the researchers said it was clear that Europe as a whole has a problem.
The study found that up to 400,000 deaths each year in the EU are directly linked to excess weight.
Of all the deaths in the UK that were linked to excess weight, about 66 per cent were down to obesity, and 33 per cent to being overweight.
In around 70 per cent of overweight-linked cases, the final cause of death was heart disease and in 20 per cent, it was cancer. Overall, around 12 per cent of heart disease deaths in Britain were due to being overweight, and 5.7 per cent of total deaths from cancer were also directly caused by being overweight or obese.
Dr Jose Banegas, who led the research, said excess weight is a major public health problem.
'One in two in the EU is obese or overweight,' he added. 'Excess weight may well come to replace smoking as the major killer of adults in the near future.
'Most countries have not yet made any systematic effort to raise public awareness as to the dangers of obesity.'
As well as being worst for fat-related deaths, the UK tops the smoking mortality league, with 21 per cent of all deaths linked to tobacco.
Obesity costs £2.6billion a year in NHS bills and indirect losses to the economy. Other studies have shown that the percentage of overweight children in Britain has virtually doubled in the last decade.
Dr Andrew Hill, of Leeds University, said the rate of adult obesity in Britain is rising by one per cent of the population a year.
Doctors say that being obese when you are 40 knocks up to seven years off your life. Obese people who smoke will die more than 13 years before their time.
Doctors are unsure why France should come out with the lowest rate of deaths due to excess weight. The French do not eat less saturated fat than the British and have similar cholesterol levels.
It has been suggested that they are protected from heart attacks by drinking alcohol, particularly red wine.
Fat families are to be prescribed a visit to their local Sainsbury's by GPs, where they will be taken by the hand and shown healthy foods.
The supermarket has struck a deal with family doctors and the drug firm Roche under which overweight patients will be offered tours of selected stores with advice from nutrition experts.
Read more

Irish teens get gastric bands as obesity time-bomb explodes
IRISH teenagers as young as 15 are being given gastric bands as the numbers needing drastic surgery continue to escalate.
Gastric bands reduce a patient's stomach size to help prevent them overeating.
Experts say it's the latest example of Ireland's spiralling obesity epidemic among the younger age group. One-in-four children are either overweight or obese in Ireland.
"I've seen kids who are of such size that they've been referred to the UK for consideration of gastric banding," explained Professor Donal O'Shea (pictured inset).
"The problem is that our treatment services are so underdeveloped that we don't have the surgery capability for obesity in children in Ireland.
"The scale of the problem in this country is on par with that in Britain.
"And we lag only a little bit behind the US, where 33pc of children are overweight, or obese.
"There has been an absolute explosion in the extreme end of obesity in kids. We have 15-year-olds in this country who weigh 16 and 17 stone.
"We've reached a stage where the argument has progressed to what is the best type of operation for children who are obese.
"I've referred two patients, aged 15 and 16, to Great Ormond Street for consideration of bariatric surgery."
Prof O'Shea, who heads the obesity management clinic in St Columcille's Hospital, Dublin, said the obesity time-bomb was no longer just ticking - it had "exploded".
He told the Irish Independent that we were fast heading towards the "nightmare scenario".
"At current trends we will need obesity surgery for more children in Ireland within the next 10 years. That's the sad reality."
Dr Sinead Murphy, consultant paediatrician in Temple Street hospital, said the obesity crisis was affecting children as young as three and four years of age. "A healthy three-year-old should probably weigh about 15 kilos. But we regularly see three-year-olds weigh 25 kilos and upwards - they are clinically obese."
Dr Murphy said children were presenting with a raft of medical problems as a direct result of their burgeoning waistlines.
"We're seeing an awful lot of muscular skeletal problems. A lot of children have joint and back pain, and breathing difficulties," she said.
"Half the kids we're seeing have high insulin levels, which means they're on a path to Type-2 diabetes.
"Half of the 10-year-olds we're seeing have high cholesterol already."
She said children eligible for bariatric surgery were given "psychological preparation" before going under the knife.
"These children could also be an anesthetic risk because they're so overweight."
Ireland's only dedicated childhood obesity treatment programme, at Dublin's Temple Street Children's Hospital, has had a 400pc increase in just one year in referrals of children aged under five.
The long-term effects of being seriously overweight include reduced educational achievement, risk of heart disease and certain cancers, as well as the possibility of developing type 2 diabetes.
"We're diagnosing diabetes in people in their 20s, and new cancers will double by 2030, driven by the obesity epidemic," said Prof O'Shea.
"We can't wait until we have to cope with kidney failure and amputation in people in their 30s and 40s."
Read more

London gastric band aftercare 2015: Address change !!!!
LONDON (10am - 03pm)
West End Medical
6 Bendall Mews
Marylebone
London NW1 6SN
AT our Weight Loss Clinic we take pride in our comprehensive after-care program which has been proven to be the most effective program for long term weight loss and weight management. As part of your after-care
- You will have access to a member of our medical team, for initial consultation or aftercare/ gastric band Fills
- You will receive full expert nutritional guidelines which are worded in a way that is easy to understand whilst still explaining every detail of the foods and drinks which you should consume along with explaining portion sizes, cooking instructions and how to re-adjust your eating habits.
- You will receive tailored exercise guidelines which are structured around your own abilities. Whatever your goal is, we will work towards it as a team!
At our Cosmetic Clinic you can have a consultation or post operative check -up with a member of our plastic surgery team Free of charge.
Read more

Dublin gastric band aftercare 2015: Address change !!!!
DUBLIN (09am - 03pm)
Harvest Moon Centre, 3d floor
24 Lower Baggot Street
Dublin 2
AT our Weight Loss Clinic we take pride in our comprehensive after-care program which has been proven to be the most effective program for long term weight loss and weight management. As part of your after-care
- You will have access to a member of our medical team, for initial consultation or aftercare/ gastric band Fills
- You will receive full expert nutritional guidelines which are worded in a way that is easy to understand whilst still explaining every detail of the foods and drinks which you should consume along with explaining portion sizes, cooking instructions and how to re-adjust your eating habits.
- You will receive tailored exercise guidelines which are structured around your own abilities. Whatever your goal is, we will work towards it as a team!
At our Cosmetic Clinic you can have a consultation or post operative check -up with a member of our plastic surgery team Free of charge.
Read more

TWO MILLION obese Brits to get free gastric band operations on the NHS
The country’s strained National Health Service could be faced with a hefty £12billion bill following the latest bid to tackle the nation’s out of control obesity crisis.
As a result of dramatic new rulings to be announced, up to two million people will be offered free weight loss surgery on the NHS.
Health watchdog NICE wants to provide more Type 2 diabetics with a free gastric band or bypass operation.
Currently, around one million people qualify for the surgery but that number will double under the new guidelines.
Critics slammed the proposals, insisting that it was “so wrong” to offer ops costing up to £6,000 each when the NHS faces a £30billion deficit.
They warned that obese people should instead be told to have a healthier diet and exercise more.
Read more

Gastric Band Aftercare clinics an prices 2015.
Belgium Surgery Services organize aftercare clinics on a regular base in several locations all over the UK, Ireland and Scotland.
All patients that require gastric band fills, defills or support are welcome to see one of our bariatric specialist.
Our gastric band aftercare prices and clinics:
- Gastric band fill / defill in London, Cardiff, Birmingham , Manchester,Glasgow, Edinburgh, Belfast: 90£
- Gastric band fill/ defill in Dublin, Killarney,Belfast : 120€
- Gastric band aftercare package UK = 5 fills for 360£
- Gastric band aftercare package Ireland = 5 fills for 480€
Read more

Weight loss surgery reduces diabetes risk
Weight loss surgery can dramatically reduce the odds of developing type 2 diabetes, according to a major study.
Doctors followed nearly 5,000 people as part of a trial to assess the health impact of the procedure.
The results, published in the Lancet Diabetes and Endocrinology journal, showed an 80% reduction in type 2 diabetes in those having surgery.
The UK NHS is considering offering the procedure to tens of thousands of people to prevent diabetes.
Obesity and type 2 diabetes are closely tied - the bigger someone is, the greater the risk of the condition.
The inability to control blood sugar levels can result in blindness, amputations and nerve damage.
Around a tenth of NHS budgets are spent on managing the condition.
Surgery
The study followed 2,167 obese adults who had weight loss - known as bariatric - surgery. They were compared to 2,167 fellow obese people who continued as they were. There were 38 cases of diabetes after surgery compared with 177 in people left as they were - a reduction of nearly 80%.
Around 3% of morbidly obese people develop type 2 each year, however, surgery reduced the figure to around 0.5%, which is the background figure for the whole population.
What is bariatric surgery?
Gastric band
Bariatric surgery, also known as weight loss surgery, is used as a last resort to treat people who are dangerously obese and carrying an excessive amount of body fat.
This type of surgery is available on the NHS only to treat people with potentially life-threatening obesity when other treatments have not worked.
Around 8,000 people a year currently receive the treatment.
The two most common types of weight loss surgery are: Gastric band, where a band is used to reduce the size of the stomach so a smaller amount of food is required to make someone feel full. Gastric bypass, where the digestive system is re-routed past most of the stomach so less food is digested to make someone feel full
The National Institute of Health and Care Excellence is considering a huge expansion of obesity surgery in the NHS in order to cut rates of type 2 diabetes.
Current guidance says surgery is a possible option for people with a BMI above 35 who have other health conditions.
But new draft guidelines argue much thinner people should be considered on a case by case basis and those with a BMI of 35 should automatically considered for surgery.
Diabetes UK says around 460,000 people will meet the criteria for an automatic assessment under the guidance.
But the total jumps nearer to 850,000 when those with a BMI of 30 are also considered, it says.
NICE anticipates figures in the tens of thousands. However, the surgery can cost between £3,000 and £15,000 and the move by NICE has raised concerns that the NHS will not be able to afford the treatment, even if there are savings in the longer term.
Obesity statistics
Crowd of people
One in four adults in England is obese
A further 42% of men are classed as overweight
The figure for women is 32%
A BMI of 30-35 cuts life expectancy by up to four years
A BMI of 40 or more cuts life expectancy by up to 10 years
Obesity costs the NHS £5.1bn every year
Source: National Institute of Health and Care Excellence
Prof Martin Gullford, from King's College London, told the BBC News website: "The key thing would be not only how effective is weight loss surgery but how safe is it in the long-term?
"And we need to know about the cost effectiveness of weight loss surgery and how that balances against the costs of diabetes, it does raise some complex issues."
Simon O'Neill, the director of health intelligence at Diabetes UK, said: "This is interesting research that reinforces what we already know about weight loss being important for both preventing and managing type 2 diabetes.
"But it must be remembered that surgery carries risks and so bariatric surgery should only be considered if serious attempts to lose weight have been unsuccessful.
"Looking at the bigger picture, as a society we also need to focus more on stopping people becoming overweight, we need to look seriously at how we can make sure people are getting support to lose weight through access to the right services to encourage them to make healthy choices."
Read more

No long-term difference after rapid or gradual weight loss
Slow and steady weight loss does not reduce the amount or rate of weight regain compared with losing weight quickly, according to research 'The effect of rate of weight loss on long-term weight management: a randomised controlled trial', published in The Lancet Diabetes & Endocrinology.
"Across the world, guidelines recommend gradual weight loss for the treatment of obesity, reflecting the widely held belief that fast weight loss is more quickly regained,” said Katrina Purcell, dietician and the first author on the paper from the University of Melbourne, Australia. “However, our results show that achieving a weight loss target of 12.5% is more likely, and drop-out is lower, if losing weight is done quickly."
The study, led by Professor Joseph Proietto, Sir Edward Dunlop Professor of Medicine at the University of Melbourne and Head of the Weight Control Clinic at Austin Health in Australia, set out to examine whether losing weight at a slow initial rate, as recommended by current guidelines worldwide, results in larger long-term weight reduction and less weight regain than losing weight at a faster initial rate in obese individuals.
The Australian trial included 200 obese adults (BMI30–45) who were randomly assigned to either a 12-week rapid weight loss (RWL) programme on a very-low-calorie diet (450–800 kcal/day) or a 36-week gradual weight-loss (GWL) programme. The GWL programme reduced participants' energy intake by approximately 500 kcal/day in line with current dietary weight loss guidelines. Participants who lost more than 12.5% of their bodyweight were then placed on a weight maintenance diet for three years.
They reported that participants who lost weight faster were more likely to achieve target weight loss with 81% of participants in the RWL group losing ≥12.5% of their bodyweight versus just 50% in the GWL group.
The researchers also found that the initial rate of weight loss did not affect the amount or rate of weight regain in these patients who entered the subsequent weight maintenance period, as similar amounts of weight were regained after three years by participants who had lost weight on either diet programme. Weight regain was around 71% in both groups after three years.
The authors suggest a number of possible explanations for their findings including that the limited carbohydrate intake of very-low-calorie diets might promote greater satiety, and less food intake by inducing ketosis. In addition, losing weight quickly may also motivate participants to persist with their diet and achieve better results.
Read more

Why choose Belgium Surgery Services for plastic surgery?
Why choose Belgium Surgery Services for plastic surgery?
In order to perform a cosmetic procedure you want to be in the hands of a doctor in whom you have 100% confidence. With us you have that security.
A plastic surgeon equipped with extensive experience.
Our plastic surgeon Dr Dedoncker performs more than 1.500 large and medium operations per year.
Your operation is performed by a certified plastic surgeon who is a member of the Royal Belgian Society for Plastic and Reconstructive Surgery. Only real plastic surgeons are members of this association.
Read more

NEW: varicose veins surgery
Belgium Surgery Services is proud to offer vascular treatments in Belgium in close partnership with Dr Robijn and the AZ Jan Portaels Hospital.
Our expertise, innovation and hard work brought our team to the world top of vascular surgery.
Read more

More weight loss operations for diabetes
An expansion of weight loss surgery in England is being proposed to tackle an epidemic of type 2 diabetes.
New draft guidelines from the National Institute of Health and Care Excellence (NICE) aim to reduce debilitating complications.
Diabetes UK estimates 850,000 people could be eligible for surgery, but NICE expects it to be tens of thousands. Type 2 diabetes is closely linked to lifestyle and obesity.
Wales and Northern Ireland are not bound by the guidance, but do tend to follow them closely. The inability to control blood sugar levels can result in blindness, amputations and nerve damage. A mounting body of evidence suggests a gastric bypass improves symptoms in around 60% of patients.
Read more

Largest European Study on Breast Implants Published
First-Ever Study on European Women: Over 1,000 Devices Monitored
London – 9 June, 2014 – Europe’s largest silicone implant manufacturer has published safety data from a five-year review* in the prestigious journal Plastic and Reconstructive Surgery (PRS), the first ever study on European women. The multi-centre study monitored 1,010 ‘Cristalline Paragel’ devices made by Eurosilicone (www.eurosilicone.com) implanted in 535 women undergoing either augmentation or reconstructive surgery. Each patient was followed up at three months post-surgery, and then annually thereafter.
Owned by Dublin-based GC Aesthetics (www.gcaesthetics.com) which is also the parent company of the UK’s only implant manufacturer Nagor (www.nagor.com), the study’s results demonstrate a reassuringly low rupture rate and an excellent safety profile for Eurosilicone’s products. This month, Eurosilicone joins its sister brand to effectively triple the variety of implant profiles and combinations available to British women, backed by the biggest cache of positive data ever researched and released. Combined, both companies produce 300,000 implants annually exported to more than 80 countries, enjoying over 60 years of history in the market.
Whilst the results don’t allow for direct comparison with competitors, the dramatically lower removal rates of implants for breast augmentation experienced by the Eurosilicone patients compared with other brands is reassuringly positive. Where implants are used in reconstructive surgery following a cancer diagnosis, Eurosilicone’s results are impressive – 50% fewer removals than its nearest competitor.
Implant removal may be required for a number of reasons and figures relating to this form a large part of the study. Most re-operations were performed for cosmetic reasons rather than reconstructive – but capsular contracture (an abnormal reaction of the body where the breast tissue forms a ‘capsule’ and hardens) was just 1.9%, while the most frequent reason for re-operation was women wanting a boob lift (mastopexy) at 10.7%, followed by scarring (3.6%). Most of the devices that were removed were associated with patients having a breast reconstruction. Out of the 365 women having a boob job – ie primary augmentation – just 4.4% had their implants removed during the five year period.
Rupture rates were exceptionally low with just one of the 1,010 implants found to be ruptured on examination. No ruptures were found during the 35 re-operations and the total risk of rupture was assessed at just 0.4% per patient.
According to GC Aesthetics’ Chief Executive Ayse Kocak, who is also the industry’s first-ever female CEO;
“This study – the largest ever published in Europe – provides very positive and reassuring news to women and surgeons worldwide, who know they can select their implants with confidence. At GC Aesthetics we are proud to be producing some of the highest quality products available, alongside the most comprehensive warranty on the market. We are thrilled to be introducing Eurosilicone to the UK, which will provide hundreds of new and reliable aesthetic possibilities to British patients.”
Eurosilicone’s product lines include the bestselling ‘Round Collection’ spanning 219 variations, as well as the ‘Matrix’ offering 9 types with 102 variations. GC Aesthetics products also offer the most comprehensive warranty on the market: free and valid for the entirety of the patients’ lifetime, rather than just the product’s lifetime.
About GC Aesthetics
GC Aesthetics, which stands for Global Consolidated Aesthetics, was founded in 2007 and is the umbrella company for two leading implant manufacturers: Nagor and Eurosilicone. The Dublin-based privately owned company has more than 60 years of combined experience and excellence in implant development, manufacture and innovation and currently manufacture and sell breast implants in 90 countries, offering a wide product range with nearly 600 types of implant. The company manufactures their products at their own facilities based in Scotland, England and France and produce to the highest European standards. GC Aesthetics is committed to the continuous improvement and evolution of the Eurosilicone and Nagor product lines and to educating consumers by providing clear information on implants.
GC Aesthetics directs group operations from their corporate headquarters in Dublin, Ireland. To contact them, please email info@gcaesthetics.com and to visit the GCA website please go to www.gcaesthetics.com
About Nagor
Nagor (www.nagor.com) is the only British manufacturer of silicone breast implants with facilities situated in Cumbernauld in Scotland and Ashby De La Zouch in central England, employing 125 highly skilled and dedicated people. They have been selling implants since 1979 and offer a lifetime patient guarantee on all breast implants.
All Nagor products are designed, developed and manufactured in facilities compliant with the ISO 13485 standards and requirements demanded for class III sterile breast implant medical devices. They are manufactured under a quality management system in accordance with ISO and EN requirements and have CE mark certification.
About Eurosilicone
Eurosilicone (www.eurosilicone.com) is a leading manufacturer in the global plastic surgery community. They are an innovative developer and manufacturer of a complete range of quality surgical implants and tissue expanders. Their extensive product line provides surgeons with a wide range of breast augmentation, aesthetic and reconstructive options.
Eurosilicone products are manufactured in state-of-the-art facilities in Apt, France. Their implants are manufactured in full compliance with ISO and EU requirements and are CE certified according to the requirements of the Medical Device Directive 93/42/EEC.
Read more

Opening new bariatric and cosmetic clinic in Killarney, Ireland
As a result of our growing excellent reputation in Obesity and Plastic surgery Belgium Surgery Services is delighted to announce the opening of our new weightloss and plastic surgery consultation clinic at Killarney, Ireland from October onwards. Our new clinic managed by Dr Maria Gordos will provide cosmetic treatments, plastic surgery consultations and weightloss managment in a highly professional and uniquely personal clinical setting.
Read more

Banding the sleeve to prevent weight regain
Laparoscopic sleeve gastrectomy is a safe and effective procedure that results in weight loss and improvements in comorbidities. Nevertheless, some patients do present with insufficient weight loss or weight regain once the initial impact and effectiveness of their LSG procedure has subsided. Professor Konrad Karcz, University of Lübeck, Germany, believes one solution to prevent failure is to employ the MiniMizer Ring (Bariatric Solutions). In an interview with Bariatric News, he discusses the indications for banded sleeve gastrectomy and the advantages for using the MiniMizer Ring.
“The gastric sleeve is gaining in popularity because it is a short and effective procedure. In the first and second year after surgery the weight loss and metabolic changes, such as resolution of type 2 diabetes, are exactly the same as a gastric bypass,” said Prof. Karcz.
Professor Konrad Karcz
In Germany, the majority of bariatric patients have BMI>45 and more than half of Prof. Karcz’s patients have a BMI>50. In his intuition, it is planned for most patients in the BMI>50 category to have a two-stage procedure: first a sleeve and if their weight loss is unsatisfactory, an additional malabsorption procedure.
“However, if the patient is on medication it is a contraindication to a malabsorption procedure, or patients may not want a second procedure,” he added. “So what do we do with patients who were not losing enough weight due to dilatation of the gastric sleeve, who cannot have a malabsorption procedure
“We realised we needed to consider additional options, such as the banding sleeve.” Prof. Karcz and his team currently use the MiniMizer Ring in the primary procedure on super obese patients and perform banded sleeve procedure on those patients who are receiving medication or who are reluctant to have a second procedure.036$
He explains that the MiniMizer Ring does not really have an impact on weight loss for the first 8-12 months, because the sleeve passage is narrower than the Ring, the device is used as a ‘preventative measure’ against the dilatation, “It is important not to make the Ring too tight at the time of the procedure, as this may cause the Ring to migrate. However, complications such as migration dislocation, infection and dysphagia are rare,” adds Prof. Karcz.
The gastric sleeve is gaining in popularity because it is a short and effective procedure.
Read more

Scientists invent the lightest-ever breast implants that will prevent your bust from sagging
A revolutionary new breast implant – the lightest ever created – is due to be introduced in Britain later this year.
The new implants, called B-Lite, will weigh 30 per cent less than any others on the market – and are designed to avoid the kind of sagging that can occur after time with conventional cosmetic breasts.
Up to now, implants have been made of weighty silicon gel or a saline water solution. The new type consists of a silicone shell filled with minute balls of silicate, a solid form of silicone gel, but much lighter.
Inventor Dael Govrin, an Israeli biochemical engineer, said: ‘Breast implants haven’t got any lighter in weight since they were first introduced in 1962. There has been no change in what goes into an implant since day one.
‘We know that after ten or 15 years, these implants will need replacing. When you put an implant in, it is a dead weight. That’s why they start to sag after a number of years and why women get through two or three sets if they want to maintain good-looking breasts.
‘We think it is important to make an implant as light as possible.’
The average conventional implant weighs just over 1lb, while the average real breast is slightly lighter than that. The new implant weighs a third less than than the conventional type.
Nearly 40 Israeli women have already been fitted with the new breasts and say they hardly notice they are there.
Mr Govrin was challenged to create the new implants by his brother Jacky, an Israeli plastic surgeon. Dael Govrin said: ‘The feedback from our first patients is extremely positive. Some of the women are having implants for the first time and they say they are lighter than their own natural breasts.
‘The breast still move naturally – from side to side – as they would if you saw a young woman on a beach walking along in a bikini. ‘Any lighter and they would have taken off. And that wouldn’t have been natural.’
Read more

Offer weight loss surgery to diabetics
An expansion of weight loss surgery in England is being proposed to tackle an epidemic of type 2 diabetes," BBC News reports. The National Institute for Health and Care Excellence (NICE) has recommended obese people with type 2 diabetes should be offered weight loss (bariatric) surgery.
These draft guidelines include new recommendations about the treatment of obesity. In particular, NICE advises that those with recent-onset type 2 diabetes who fulfil certain body mass index (BMI) criteria should have surgery. The recommendations also provide guidance on the use of very low-calorie diets.
As is often the case, the proposed NICE recommendations have made a huge media splash, leading to front-page headlines such as the Daily Mail's claim that, "Thousands more to get obesity ops on the NHS".
These are draft guidelines, so it is far from certain whether they will become official advice. A consultation will be taking place between July 11 and August 8 2014.
Diabetes and obesity – a deadly combination
NICE is focusing on people who are obese and have diabetes because the combination of these two conditions can be particularly dangerous.
Complications of diabetes can include:
- heart disease
- stroke
- nerve damage
- eye damage
- kidney disease
What are the main new draft guidelines?
Currently, bariatric surgery is offered to people with a BMI of 40 or more, or those with a BMI between 35 and 40 if they also have another significant and possibly life-threatening disease that could be improved if they lost weight, such as type 2 diabetes or high blood pressure.
Patients must have tried and failed to achieve clinically beneficial weight loss by all other appropriate non-surgical methods and be fit for surgery. This recommendation has not changed.
The updated draft guidelines include additional recommendations on bariatric surgery for people with recent-onset type 2 diabetes. These recommendations include:
- Offering an assessment for bariatric surgery to people who have recent-onset type 2 diabetes and are also obese (BMI of 35 and over).
- Considering an assessment for bariatric surgery for people who have recent-onset type 2 diabetes and have a BMI between 30 and 34.9. People of Asian origin will be considered for surgery if they have a lower BMI than this, as the point at which the level of body fat becomes a health risk varies between ethnic groups. Asian people are known to be particularly vulnerable to the complications of diabetes.
What is bariatric surgery?
Bariatric surgery includes gastric banding, gastric bypass, sleeve gastrectomy and duodenal switch.
A range of techniques are used, but they are usually all based on the principle of surgically altering the digestive system so it takes less food and makes the patient feel fuller quicker after eating.
The two most common types of weight loss surgery are:
- gastric band – where a band is used to reduce the size of the stomach so a smaller amount of food is required to make someone feel full
- gastric bypass – where the digestive system is rerouted past most of the stomach so less food is digested, which makes the person feel full
These procedures are usually performed using keyhole surgery.
What are the risks?
As with all types of surgery, weight loss surgery carries a risk of complications. These include:
- internal bleeding
- a blood clot inside the leg (deep vein thrombosis)
- a blood clot or other blockage inside the lungs (pulmonary embolism)
It is estimated the risk of dying shortly after gastric band surgery is around 1 in 2,000. A gastric bypass carries a higher risk of around 1 in 100.
The surgery also carries the risk of other side effects, including:
- excess skin – removal of excess skin is usually considered a form of cosmetic surgery, so it is not usually available on the NHS
- gallstones – small stones, usually made of cholesterol, that form in the gallbladder
- stomal stenosis – where the hole that connects the stomach to the small intestine in people with a gastric bypass becomes blocked
- gastric band slippage – where the gastric band slips out of position
- food intolerance
- psychosocial effects – for example, some people have reported relationship problems with their partner because their partner begins to feel nervous, anxious or possibly jealous of their weight loss
What other treatments have new draft recommendations?
The draft guideline also makes recommendations regarding very low-calorie diets (800kcal per day or less). These include:
- Not routinely using very low-calorie diets to manage obesity.
- Only considering very low-calorie diets for a maximum of 12 weeks (continuously or intermittently) as part of a multicomponent weight management strategy with ongoing support. This would be for people who are obese and have a clinically assessed need to rapidly lose weight – for example, people who require joint replacement surgery or who are seeking fertility services.
- Giving counselling and assessing people for eating disorders or other mental health conditions before starting them on a very low-calorie diet. This is to ensure the diet is appropriate for them.
The risks and benefits of surgery should also be discussed. Patients should be made aware that very low-calorie diets are not a long-term weight management strategy and that regaining weight is likely, but not because of a failure on their or their clinician's part.
How were the draft recommendations received?
There is concern about how many people will be eligible for treatment under the new guidelines and how much it will cost, with Diabetes UK estimating that 850,000 people could be eligible for surgery.
Simon O'Neill, from the charity Diabetes UK, has been quoted as saying that, "Bariatric surgery should only be considered as a last resort if serious attempts to lose weight have been unsuccessful and if the person is obese.
"It can lead to dramatic weight loss, which in turn may result in a reduction in people taking their type 2 diabetes medication, and even in some people needing no medication at all.
"This does not mean, however, that type 2 diabetes has been cured. These people will still need to eat a healthy balanced diet and be physically active."
What is the rationale behind the new recommendations regarding bariatric surgery?
Professor Mark Baker, director of the Centre for Clinical Practice, said that, "Updated evidence suggests people who are obese and have been recently diagnosed with type 2 diabetes may benefit from weight loss surgery.
"More than half of people who undergo surgery have more control over their diabetes following surgery and are less likely to have diabetes-related illness; in some cases, surgery can even reverse the diagnosis. The existing recommendations around weight loss surgery have not changed."
It could actually be the case that increasing access to bariatric surgery will save the NHS money in the long term if this helps combat the obesity epidemic.
If obesity levels continue to rise at their current rates, it is estimated that by 2050 the annual cost of treating obesity-related complications will be £50 billion, more than half the entire current NHS budget for England.
One million operations at £5,000 each – £5 billion in total – could well seem a bargain in comparison.
Read more

Bariatric surgery yields higher diabetic remission
Stomach-shrinking bariatric surgery beats other forms of treatment in bringing about remission of type 2 diabetes in the obese, according to a Swedish study out Tuesday.
The study, to appear in Wednesday's issue of the Journal of the American Medical Association (JAMA), also found that the procedure was linked to fewer diabetes-related complications in the severely overweight.
The findings come at a time when obesity and diabetes have reached epidemic proportions, creating a costly public health problem.
In the United States, more than 29 million people -- or 9.3 percent of the population -- had diabetes in 2012, up from an estimated 26 million two years earlier, the Centers for Disease Control and Prevention said Tuesday. Treating the disease and related complications amounted to $245 billion in medical expenses, as well as lost pay in 2012, up from $174 billion five years earlier.
Carried out by a team led by Lars Sjostrom of the University of Gothenburg, the findings to appear in JAMA involved a follow-up of the Swedish Obese Subjects study.
The median follow-up time was 18.1 years for people who had had surgery and 17.6 years in the control group in an effort to determine the long-term effects of bariatric procedures, diabetes remission and diabetes-linked complications.
The authors found that the proportion of people with type 2 diabetes who had bariatric surgery and were in remission was 72.3 percent two years after the procedure, compared to 16.4 precent in the control group.
Fifteen years on, the diabetes remission rates were 30.4 percent for those who had surgery, significantly higher than the 6.5 percent remission in the control group.
All kinds of bariatric surgery -- including gastric bypass and adjustable and nonadjustable banding procedures -- "were associated with higher remission rates compared with usual care," said a release announcing the study.
What's more, according to the authors who say the findings require confirmation through randomized trials, this type of surgery is also linked to a lower incidence of micro- and macrovascular complications.
According to Tuesday's CDC data, one in four people with diabetes in the United States aren't aware they have the disease. What's more, 86 million US adults aged 20 and older have what is known as prediabetes -- that's when blood sugar levels are above normal but not high enough to be deemed type 2 diabetes.
Without shedding pounds and engaging in moderate physical activity, 15 to 30 percent of this at risk group could develop the full-blown disease within five years, the CDC warned. It said 208,000 people younger than 20 have been diagnosed with type 1 and type 2 diabetes.
"These new numbers are alarming and underscore the need for an increased focus on reducing the burden of diabetes in our country," said CDC official Ann Albright. "Diabetes is costly in both human and economic terms. It's urgent that we take swift action to effectively treat and prevent this serious disease."
Read more

'Gummy Bear' Breast Implants: The Future of Breast Augmentation Surgery?
Like kids in a candy store, more women are seeking out a type of silicone breast implant that one doctor calls the "gummy bear."
Dr. Grant Stevens, a prominent plastic surgeon in Marina Del Rey, Calif., coined the term "gummy bear breast implant." He said he gave the implants their catchy nickname because when cut in half, the implant is stable and retains its shape, much like the chewy, gummy bear candies.
Stevens is an advocate of the "gummy bears" because he said he believes they look and feel more like natural breasts. He insisted that "gummy bears" are also safer than other types of implants because they have a lower rupture rate.
"The 'gummy bear' breast implants are new to Americans," Stevens said. "They're cohesive gel, and they're form-stable. They keep their shape."
These new "high-strength silicone gel implants" made by a company called Sientra were approved in March by the U.S. Food and Drug Administration. But neither the agency nor the company call them "gummy bears."
"We do not condone the use of such terms," Sientra CEO Hani Zeini told "Nightline" via email.
Zeini said equating a medical device to a piece of candy trivializes it, and FDA officials are inclined to agree.
Breasts are big business in the United States, with about $1 billion spent on cosmetic breast surgery a year. According to the American Society of Plastic Surgeons, more than 300,000 American women undergo cosmetic breast augmentation every year -- up 45 percent since 2000.
Improvements in breast implant technology have had a huge impact on the market in the past. Over the past 15 years, since silicone implants became widely available in the U.S., the number of cosmetic procedures has tripled.
For years, this type of high-strength silicone gel breast implant was only available to patients in the U.S. who were willing to take part in clinical trials through surgeons like Stevens.
For some patients, it's their second breast augmentation surgery. Aubrie Chacon said she wanted to get her breast implants redone because her current ones felt like "weird water" under her skin.
"I would like something that felt more natural," she said. "Not so fake, not so foreign."
Christy Carlton, another one of Stevens's patients, said she got her Sientra breast implants through a clinical trial six years ago, and hasn't had any problems since. She added that her partner didn't know that she had breast augmentation surgery until she told him because she said her breasts looked and felt so natural.
But breast surgery is a sensitive subject. In most cases, it's totally elective and, of course, it is closely tied to the patient's self image. Plus, when any new product is introduced, there is a real issue of safety and there have been problems in the past.
Read more

How best friends' matching gastric band operations turned them into 'Little and Large'
Best pals Lisa and Claire did everything together, especially eating their favourite fatty foods.
Over nearly two decades of friendship they slowly ballooned in size until 5ft 4ins Lisa became a 16-stone size 20 and 5ft 9in Claire was a 20-stone size 24.
They both kept trying diets without success and with her 40th birthday close Lisa decided on drastic action. When the day dawned she was sitting in a consultant’s room planning gastric band surgery. By her side, as always, was Claire.
Inspired by her pal’s example, she also booked in to have surgery and a month later they were lying in side-by-side hospital beds in Belgium.
http://www.mirror.co.uk/news/real-life-stories/gastric-band-mishaps-left-friends-3215460#ixzz325qjcicD
Follow us: @DailyMirror on Twitter | DailyMirror on Facebook
Read more

New ‘Internal Bra’ Promises Permanent Push-Up
A new breast lift procedure acts like an implanted push-up bra for women undergoing breast lift or breast reduction surgery.
The Orbishape system is like a sling for breast tissue that gets surgically tethered to the rib cage by silicone threads and titanium screws.
“Think of it as a hammock that sits underneath your breast to keep it supported, or like the bottom part of an underwire bra,” said Yossi Mazel, the chief operating officer of Orbix Medical, a medical device company based in Tel Aviv, Israel.
Related: Gummy Bear Breast Implants
Mazel said that traditional breast lifts often begin to sag within months, but the Orbishape helps preserve the results of surgery by providing additional support. In trials, breasts remained perky for at least five years, he said, adding that the implant isn’t intended to be a stand alone procedure.
The “internal bra” also helps patients heal faster and reduces the appearance of surgery scars, Mazel said. It doesn’t interfere with mammograms.
The new device, which is approved for use in some European countries, will undergo review by the Food and Drug Administration for use in the U.S. sometime later this year, Mazel said. The cost of the device, if approved, is unclear, but insurance companies might pick up the tab for breast cancer patients undergoing reconstructive surgery.
Read more

Free consultation breast augmentation
Free consultation Breast implants
If you are unhappy with the shape of your breasts then surgery may be a solution for you. Belgium Surgery Services is the Number 1 in BELGIUM for breast surgery. We’ve performed over 4000 surgeries over the past 10 years at our hospital.
If you are considering surgery, your first step will be a free consultation to evaluate your needs and concerns and to discuss the broad range of options available to you.
Book your consultation on www.belgiumsurgeryservices.com and meet one of our experts in your home country.
Expertise at Affordable Prices 2850€
Our priority is a beautiful result, performed by experts in the art of breast augmentation and we use silicone implants with life time guarantee.
Our prices are all inclusive: consultation, operation, taxiservices between airport, hotel and hospital , 2 nights hotel *** , personalcoaching and free aftercare.
Reasons to consider Breast Surgery
- Find a new confidence in your body
- Increase the beauty, shape and size of your breasts
- Enhance the proportions of your body
- Correct loss of shape from pregnancy or breast feeding
- Restore breasts to a youthful and perky shape
- Repair, replace or improve past breast surgery
- Repair the breast to its natural beauty following mastectomy
- Wear the clothes you want to!
Read more

Bariatric surgery can reduce liver damage
Bariatric surgery can result in significant improvement in nonalcoholic fatty liver disease (NAFLD), according to new research presented at Digestive Disease Week (DDW). Researchers at the University of South Florida-Tampa (USF) found that bariatric surgery resolved liver inflammation and reversed early-stage liver fibrosis, the thickening and scarring of liver tissue, by reducing fat deposits in the liver.
Dr Michael Murr
"About 30 percent of the US population suffers from this disease, which is increasing, and more than half are also severely obese," said Dr Michel Murr, lead researcher of the study, professor of surgery and director of Tampa General Hospital and USF Health Bariatric Center. "Our findings suggest that providers should consider bariatric surgery as the treatment of choice for NAFLD in severely obese patients."
Murr and his colleagues suggest that bariatric surgery be considered for patients with a BMI>35 and obesity-related co-morbidities or BMI>40. They note that traditional interventions, such as medications, have a low success rate with these patients.
Researchers compared liver biopsies from 152 patients, one at the time of the bariatric procedure and a second an average of 29 months afterwards. Mean pre-op BMI was 52±10 and mean excess body weight loss was 62±22% at the time of the subsequent biopsy.
In examining pre-operative biopsies, researchers identified patients with cellular-level manifestations of NAFLD, specifically, fat deposits and inflammation of the liver. These types of liver damage can lead to liver fibrosis and cirrhosis.
After reviewing post-operative biopsies, they found that bariatric surgery resulted in improvements for these patients. In the post-operative biopsies, researchers found that fat deposits on the liver resolved in 70 percent of patients. Inflammation was also improved, with lobular inflammation resolved in 74 percent of patients, chronic portal inflammation resolved in 32 percent, and steatohepatitis resolved in 88 percent.
In addition to these improvements, 62 percent of patients with stage two liver fibrosis had an improvement or resolution of the fibrosis. One of three patients with cirrhosis also showed improvement.
Murr noted that these findings on fibrosis reversal apply only to early-stage fibrosis, and not late-stage liver disease.
"We are in the midst of an obesity epidemic that can lead to an epidemic of nonalcoholic fatty liver disease," added Murr. "As a tool in fighting obesity, bariatric surgery could also help prevent the emergence of widespread liver disease."
Read more

Changes in appetite after bypass aids weight loss
It has been known for some time that changes in appetite, taste and smell are par for the course for people who have undergone Roux-en-Y gastric bypass surgery however, a UK study has found that patients who experienced food aversions enjoyed significantly more postoperative weight loss and reduction in their BMI compared to their counterparts without such dislikes.
The study by researchers from Leicester Royal Infirmary, UK, stated that patients frequently report sensory changes after gastric bypass surgery and these changes could lead to further weight loss.
The paper, published in the journal Obesity Surgery, indicates that subjective changes in appetite, taste and smell are very common after Roux-en-Y gastric bypass, and patients should be routinely counselled about these changes as part of the informed consent process for surgery.
It is apparent from day-to-day practice that patients frequently report changes to their appetite, taste and smell after weight loss surgery. There has been surprisingly little written in the literature on this. The aim of the study was to assess these parameters in a cohort of patients undergoing Roux-en-Y gastric bypass surgery.
The research team sent questionnaires out to patients who had undergone the procedure at the University Hospitals of Leicester between 2000 and 2011. In total, 103 patients answered the 33 questions about appetite, taste and smell set to them.
Of the respondents, almost all (97 percent) reported changes to their appetite after having the surgery. Their experiences varied, with subjects reporting that their sense of smell and taste were either unchanged, heightened or reduced. Forty-two percent of respondents said their sense of smell changed and 73 percent of patients noted change in the way food tasted, and especially in their sweet and sour palate. Respondents especially noted a change in the taste of chicken, beef, pork, roast meat, lamb or sausages, while fish, fast foods, chocolate, greasy foods, pasta and rice were also high on the list.
Three out of every four (73 percent) patients noted that they had developed an aversion to specific foods after the surgery. Meat products topped the list, with one in every three patients steering away from chicken, minced beef, beef steak, sausages, lamb, ham or bacon.
Starches such as pasta, rice, bread and pastry and dairy products such as cream, ice cream, cheese and eggs were a no-no for almost 12 percent of respondents. Only 4 percent of respondents reported having an aversion for vegetables, 3 percent for fruit, and 1 percent for tinned fish.
Interestingly, patients who experienced food aversions enjoyed significantly more postoperative weight loss and reduction in their BMI compared to their counterparts without such dislikes. They typically experienced weight loss of around 8 kilograms and a loss of BMI of 3 kg/m2 greater than their counterparts.
It is still unclear what the role is that perceptual changes in the taste and smell of food play to influence calorie intake, meal composition and subsequent weight loss following bariatric surgery. However, the researchers believe the sensory changes are due to a combination of gut hormone and central nervous system effects.
Read more

Cousin Biotech launches BIORING iPhone App
Cousin Biotech has launched its new BIORING iPhone App for patients with a BIORING gastric band. The company believes that the patient is the key to the success of a bariatric procedure, therefore it is fundamental to ensure a good follow up of the patient and assist them in their day-today lives.
As a result, Cousin Biotech decided to closely work with Ms Sally Norton, consultant bariatric surgeon and British Obesity and Metabolic Surgery Society (BOMSS) council member, to develop an App dedicated to patient, addressing this problem and improving patient safety.
“After 13 years treating and supporting gastric band patients it is clear to us that good preparation, understanding and follow-up are really important for long-term success,” said Ms Norton. “In addition, making changes to the mind-set around eating behaviour and activity are vital. Mobile phone apps are an increasingly popular way of providing information at your fingertips. We have therefore developed a mobile phone app to help support patients before and after gastric banding.”
The app enables patients to record all of the details of their surgery and band fills, to chart their progress and to advise them in case of any problems with their band. In addition, it provides advice on how to change behaviour to get the best from their gastric band.
“Equally valuable, and based on our extensive experience, is a check list to help patients decide if a fill is really required, and innovative meal and eating timers to help patients eat slowly to reduce potential problems in the future,” she added. “This app was designed to help ensure a safe and successful outcome after gastric band surgery by supporting patients in their weight loss journey.”
The app is iPhone and iPad compatible with a IOS 7 version minimum, and is now available for FREE on the App Store.
Read more

FXR receptor key to success of sleeve gastrectomy
The therapeutic value of vertical sleeve gastrectomy is not a result of the mechanical restriction of a smaller stomach but the result of increased circulating bile acids that are known to bind to the nuclear receptor farsenoid-X receptor (FXR), according to researchers from the University of Cincinnati (UC), the University of Gothenburg, Sweden, and Cincinnati Children's Hospital Medical Center.
Randy Seeley
"There are very large debates over how small to make the sleeve," said co-principal investigator, Dr Randy Seeley, professor in the endocrinology, diabetes and metabolism division at UC and director of the Cincinnati Diabetes and Obesity Center. "Conventional thought is when you make the stomach smaller, patients lose more weight because they have less room to put more food and, therefore, eat fewer calories. But as it turns out, the reason why the surgery works is that you are changing the bile acids."
The research, 'FXR is a molecular target for the effects of vertical sleeve gastrectomy' was published online in Nature, showed that following vertical sleeve gastrectomy, there is a change in bile acids that bind to a nuclear receptor called FXR. In the absence of FXR, weight-loss success and improvement in diabetes from vertical sleeve gastrectomy was reduced.
Although substantial changes in circulating total bile acids are known to occur after sleeve gastrectomy and bile acids are known to regulate metabolism by binding to the nuclear receptor FXR (farsenoid-X receptor, also known as NR1H4), the underlying molecular mechanisms are unknown.
As a result, the researchers examined the results from sleeve gastrectomy applied to mice with diet-induced obesity and targeted genetic disruption of FXR. Despite having a smaller sleeve, the rodents without the FXR receptor did not lose weight.
Because bile acids and FXR receptors interact with gut microbial communities, the researchers also looked at gut bacteria after sleeve gastrectomy. They found that the surgery also results in changes in the gut bacteria.
"Importantly, we observed changes in several key bacterial groups that have been previously linked to the risk of Type 2 diabetes, and these changes were related to FXR and bile acids," said Dr Karen Ryan, lead author and assistant professor of endocrinology, diabetes and metabolism at UC.
"Manipulating the gut bacteria is another way we think that we might be able to mimic how surgery works without having to do the cutting and stapling," said Seeley. "There are not enough surgery tables or surgeons to treat the obesity epidemic, so we need to understand how bariatric surgery works so that we can offer more scalable solutions.”
This work was supported by grants from the UNIK Food Fitness and Pharma for Health and Disease research programme, the Torsten Söderberg and Novo Nordisk foundations, Ethicon Endo-Surgery, and the National Institute of Health’s National Institute of Diabetes and Digestive and Kidney Diseases and National Heart, Lung and Blood Institute
Read more

Tameside one of UK's fat capitals
Tameside is one of the UK's fat capitals, new figures have revealed.
More than two thirds of Tamesiders are overweight or obese, according to figures from Public Health England.
They show that 69.2 per cent of people in Tameside have a body mass index (BMI) of 25 or more – one of the worst rates in Greater Manchester.
The borough shared the 33rd place with two other areas out of a list of 326 local authorities, which ranks areas from the highest to the lowest percentage.
It comes just a year after the British Heart Foundation said people who live in the borough are more likely to die from coronary disease than anywhere else in the UK.
Health chiefs are calling for action - saying obesity is now the biggest threat to health locally.
Dr Kailash Chand, chairman of Healthwatch Tameside and deputy chairman of the British Medical Association said: “The statistic is alarming and worrying.”
“Unless we get a grip of this public health emergency I believe it will cripple the NHS and the health of our borough to the point of no return.”
And while national statistics show that Copeland in west Cumbria was named the most obese town in the country with 75.9 per cent of residents having an unhealthy BMI.
In Greater Manchester, only Oldham was only marginally worse, with 69.6 per cent.
Tameside was followed by Rochdale (68.6 per cent) while Trafford ranked the healthiest with just over half (59.7 per cent) of people classed as overweight.
Nationally, Kensington and Chelsea in London was the slimmest local authority, with just 45.89 per cent of people ranked as too heavy.
Dr Chand blamed the health crisis on poor diet adding: “One of the real culprits is the amount of sugar we consume in fizzy drinks and processed food.
“About 40 to 50 per cent of all consultations in GP practices are as a direct consequence of diet-related illness like a new diagnosis of Type 2 diabetes or its complications - heart disease, stroke, certain type of cancers and kidney failure.
“All GPs and primary healthcare professionals need to proactively discuss weight management with patients, routinely measure children’s height and weight, and check adult waist circumferences as an indicator of abdominal obesity.”
Andrew Gwynne, Labour MP for Audenshaw, Denton and Dukinfield , and a shadow health minister, said: “These findings should shock us out of our complacency.
“It is clear that the current voluntary approach is not working and we need to open our minds to new approaches in tackling obesity.
“Helping parents in places like Tameside to protect and promote the future health of our children is exactly what we need to be doing.”
Read more
_ove4.png)
Bariatric Surgery Cuts Uterine Cancer Risk by 71 Percent, Researchers Find
TAMPA, Fla. -- Obese women who maintained weight loss after bariatric surgery seemed to have a 71% lower risk of developing uterine cancer as compared with women who were obese and did not undergo surgery, investigators reported here.
Overall, obesity almost tripled the risk of uterine cancer as compared with non-obese women. The cancer risk posed by obesity declined sharply in the subgroup of women who had bariatric surgery and remained significantly lower in patients who kept the weight off versus those who did not (RR 0.29, 95% CI 0.27-0.32).
The retrospective analysis of data does not prove that bariatric surgery reduces the risk of uterine cancer but does add to a growing body of evidence that obesity increases a woman's risk of the cancer, Kristy Ward, MD, said during a presentation at the Society of Gynecologic Oncology meeting.
"A history of bariatric surgery is associated with a substantial and clinically significant reduced risk of uterine cancer," said Ward, of the University of California San Diego. "Our previous work, in agreement with the findings of others, has indicated that the risk of uterine malignancy increases linearly with BMI [body mass index].
"Along with the findings of this current study, this supports that obesity may be a modifiable risk factor related to development of endometrial cancer."
Multiple studies have shown significant associations between obesity and various types of cancer. Among gynecologic malignancies, endometrial cancer has the strongest association with increasing body mass, estimated at about 40% of all endometrial cancers.
Proving that weight loss reduces cancer risk has been difficult, said Ward, as many patients regain weight over time, complicating long-term follow-up needed to study cancer. Observational studies have suggested a reduced risk of breast cancer after intentional weight loss.
Bariatric surgery leads to rapid and substantial weight loss, which tends to be greater and more durable as compared with other methods of weight loss, Ward continued. Good evidence supports resolution of diabetes and cardiovascular risk factors following bariatric surgery. Evidence of a reduced cancer risk is more modest but continues to accumulate.
Ward and colleagues hypothesized that the risk of uterine malignancy would be reduced in women who had a history of bariatric surgery. To test the hypothesis, they reviewed admission records in the nationwide University HealthSystem Consortium database, limiting the search to the time frame of Jan. 1, 2009, to June 1, 2013.
The query produced records for 7,431,858 admissions, including 103,797 patients with a history of bariatric and 44,345 cases of uterine cancer. Investigators separated the patients into currently obese and non-obese groups and further divided them into groups who had a history of bariatric surgery and those who did not.
Overall, non-obese women with a history of bariatric surgery had the lowest risk of uterine cancer at 270/100,000 admissions. Non-obese women without a history of bariatric surgery had the second lowest risk at 496/100,000 admissions.
Among obese patients, those with a history of bariatric surgery had a uterine cancer rate of 682/100,000 admissions, and obese women without a history of bariatric surgery had the highest risk at 1,409/100,000 admissions.
Investigators then calculated the relative risk of uterine cancer as compared with women who were obese and had no history of bariatric procedures. Non-obese women without a history of bariatric surgery had an 81% lower risk (RR 0.19), followed by non-obese women with a history of bariatric surgery (RR 0.29).
Women who were obese despite having undergone bariatric surgery still had 52% lower risk of uterine cancer versus women who were obese and had no history of bariatric procedures (RR 0.48).
Asked to address the potential underlying biologic mechanisms by which bariatric surgery might reduce uterine cancer risk, Ward said the mechanism remains undetermined, but some evidence suggests the surgery reduces inflammation, which is known to play a role in cancer evolution.
In response to another question from the audience, Ward said the investigators did not have the individual patient data needed to evaluate uterine cancer risk by type of bariatric surgery procedure.
Read more

UK experts publish guide for commissioning Tier 3 services
Healthcare experts in the UK have published a clinical commissioning guide on weight loss services to assist Clinical Commissioning Groups (CCGs) in commissioning these services and reduce variation in access to weight-loss clinics across the country.
The guidance was developed following a National Institute for Health and Care Excellence (NICE) accredited process and has been welcomed healthcare professionals across several disciplines. It has the backing of five Royal Colleges, the British Obesity and Metabolic Surgery Society (BOMSS), the Faculty of Public Health, the National Obesity Forum (NOF), the British Dietetic Association (BDA) and the British Psychological Society.
Mr Richard Welbourn
“The Royal College of Surgeons and BOMMS have developed a commissioning guide for Tier 3 services which covers weight assessment and management which takes into account the views of ten sponsoring organisations,” said Mr Richard Welbourn, Consultant Surgeon and President BOMSS and Professor John Wass, academic vice-president at the Royal College of Physicians (RCP). “The guide includes input from patients, pathologists, bariatric physicians, general practitioners, public health experts, dieticians, psychologists and healthcare commissioners. It deals with the roles of the weight management clinic, the multidisciplinary team, the role of general practitioners, the role of the clinic itself, referral to bariatric surgery and peri- and post-operative care.”
Although Tier 3 obesity services offer support from clinicians, specialist dietician, psychologist and exercise specialists and are a prerequisite for patients seeking Tier 4 services such as bariatric surgery, surgeons, physicians and other health professionals have been concerned that access to Tier 3 weight management clinics is restricted in some parts of the country.
A lack of provision of Tier 3 obesity services in some parts of the country was highlighted by the Royal College of Surgeons in January 2014 pointing out that it risked leaving obese patients unable to access vital services they need to help control their weight.
Recently, Public Health England and NHS England published a report, which sought to clarify responsibility for providing Tier 3 obesity services and recommended that they should be commissioned by CCGs.
This new guide sets out how those services should be commissioned.
Recently published Hospital Episodes Statistics data shows there has been a fall of 10% in the number of bariatric surgical procedures being performed between April 2012 and March 2013, even though the most recently available statistics show obesity rates in England continuing to rise.
“We hope that this guidance will clarify the role of Tier 3 services in helping patients with weight problems,” they added. “We are aware that Tier 3 services need to be developed in a number of areas in the UK. We believe that the service model set out in this guide should be adopted as quickly as possible across the country to ensure that a consistent service is provided to those who need it.”
BOMSS is the sponsoring organisation and the guidance is supported by the Royal College of Surgeons, Royal College of Physicians, the Royal College of General Practitioners, the Royal College of Pathologists, the Royal College of Psychiatrists, The British Dietetic Association, the National Obesity Forum, The Psychological Society and the Faculty of Public Health.
Read more

Bypass can alleviate knee pain in obese patients
Gastric bypass surgery could alleviate knee osteoarthritis (OA) in obese patients according to the results of a study (The Impact of Gastric Bypass Surgery Compared to Total Knee Arthroplasty on Knee Symptoms), presented at the 2014 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS).
The study involved two groups of patients: 20 of the participants (16 women and four men) had undergone gastric bypass surgery and 40 participants underwent total knee replacement for symptomatic knee osteoarthritis. The participants were on average 52 years old and had a mean pre-operative BMI 45.6.
Researchers said the participants were matched two-to-one by age, gender and BMI. The study assessed knee symptoms before surgery, six months after surgery and a year after surgery.
Bariatric surgery patients reported significant improvement in mean knee pain (6.95 vs. 2.30 points) and physical function (21.5 vs. 7.05) at one-year follow up. When compared to patients who underwent TKR, the %age improvement in mean pain scores was similar between the two groups at six months (49.9% versus 58.3%) and one year (62.7% vs. 68.2%). The bypass group experienced a significantly greater %age improvement in physical function at six months (66.3% vs. 46.7%), and a similar, though marginally non-significant difference at one year (68.4% vs. 51.5%).
Comparatively, bypass patients with self-reported OA had greater knee pain and worse function preoperatively when compared to those without OA, as well as a smaller percentage improvement in pain (63.5% vs. 74%) and function (66.4% versus 72.9%) at final follow up.
The study authors recommend that surgeons consider bariatric consultation for obese patients who have knee symptoms but lack advanced osteoarthritis or other conditions amendable to orthopaedic management.
Read more

Obesity down to living close to takeaways
By Jane Kirby – 15 March 2014 03:30 PM
PEOPLE who live or work near takeaways eat more junk food and are almost twice as likely to be obese as those who have none on their doorstep, a study has found.
Consumers who are the most tempted by takeaways and fast food eat an extra 40g of high calorie food – the same as half a small serving of McDonald's fries – every week compared with those who stay away.
Working near a fast-food place or takeaway caused the biggest problems, closely followed by them being located near the home.
The research, published online in the British Medical Journal (BMJ), is the first UK study to combine data from home, work and commuting and involved 5,442 adults from Cambridgeshire aged 29 to 62.
Read more

What are the most popular cosmetic surgery procedures for women?
In the UK, women accounted for 90.5% of all cosmetic procedures in 2013 with a total of 45,365 procedures.
Breast augmentation was the most popular with 11,123 surgical procedures carried out in 2013 - a rise of 13% on the previous year. Blepharoplasty (eyelid ops) were the second most popular cosmetic procedure followed by face or neck lifts in third place.
Liposuction procedures saw the biggest increase - 3,772 procedures were performed in 2013 (an increase of 43% since 2012). Although none of the top ten surgical procedures for women recorded a decrease, some did see a slight decline in popularity; abdominoplasty dropped from sixth most popular in 2012 to seventh in 2013 and fat transfer procedures have dropped from seventh place to eighth.
Read more

15 years of the mini-gastric bypass
MINI-GASTRIC BYPASS (MGB) is an effective, relatively low-risk and low-failure procedure, according to 15-year outcomes from 6,385 consecutive cases.
Presenting the outcomes at the IFSO meeting in New Delhi, Dr Robert Rutledge, Nevada, said that these results add to the growing evidence that MGB is a safe and effective procedure with many of the features of an ideal bariatric surgery.
From September 1997 to June 2011, 6,385 patients underwent MGB, with the mean pre-operative weight (+/- standard deviation) was 143 +/-31kg, BMI 47+/-7; 83% of the patients were female.
Outcomes
The mean operative time was 41 minutes and median length of stay was one day. Early complications occurred in 4.9% of the patients; 44 patients (0.7%) had anastomotic leaks. Three patients (0.05%) presented with dypepsia/bile reflux that was not responsive to medical therapy and were successfully treated by Braun side-to-side jejuno-jejunostomy.
Gastritis/dyspepsia/marginal ulcer was the most serious long term complication; routinely treated medically. Three deaths (0.05%) occurred within 30 days of surgery. The most recent death was in 2004.
Weight loss
Excessive weight loss occurred in 1% of patients; treated by take down of the bypass. The mean percent excess weight loss was 78% and the ten-year weight regain, 4.9%. At 18 months, 95% of patients achieved >50% EWL and 92% at 60 months. Inadequate weight loss or significant weight regain was found in 6% of patients and these patients subsequently underwent a revision (addition of ~2 meters to the bypass). Rutledge said that these reported outcomes are comparable to other large, long term MGB series reported in the literature (Obes Surg. 2012 22(5):697-703).
Comparable procedures
In addition, Rutledge also presented the preliminary results from an IFSO Varianational Committee on New Procedures Survey that interviewed over 118 surgeons from 30 countries and who shared their career experience from over 39,000 bariatric cases. The surgeons were asked their expert opinion on laparoscopic gastric banding, sleeve gastrectomy,
Roux-en-Y gastric bypass (RNY) and MGB.
Asked whether weight gain was common after each procedure, all experts agreed that weight gain was common after banding, 42% said weight gain was common after sleeve, 39% said weight gain was common after RNY bypass and only 9% said weight gain was common after MGB.
When asked the converse question regarding major weight loss, 10% said major weight loss was common after banding, 78% said it was common after sleeve, 84% said it was common after bypass and 90% said it was common after MGB. Over 90% said that banding presented a risk of post operative acid reflux, 60% said the sleeve presented a risk of post op acid reflux, but only 5% said RNY bypass presented a risk of reflux, while 10% said MGB presented a risk of reflux. This is important because extensive data show that acid reflux can lead to oesophageal cancer.
Finally, when asked about the ease of revision surgery, 30% agreed that banding revision was easy, 52% agreed that sleeve revision was easy, 22% agreed that bypass revision was easy, while 90% said MGB agreed that sleeve revision was easy. “These 15 year data confirm other studies showing that the MGB is comparable, and in some instances preferable, to more common procedures such as banding, RNY bypass and sleeve,” concluded Rutledge. “In spite of initial scepticism, MGB is a safe and effective procedure and can be easily revised, converted or reversed.”
Read more

Obese people in Wales 'denied' life saving treatment
Obese people in Wales are being denied access to life saving treatments, a leading group of surgeons has said.
The British Obesity and Metabolic Surgery Society has said morbidly obese people have been told to gain weight to qualify for bariatric surgery.
It voiced its concerns to the Welsh government's health and social care committee. The Welsh government said new criteria for surgery would be introduced soon following a review in 2013. The latest government figures show 59% of adults in Wales are classed as overweight or obese.
Read more

Gastric bypass surgery has sustained improvement in cardio risk
Bariatric surgery can result in a significant reduction in a patient’s ten year cardiovascular risk, according to two studies presented at this year’s Annual Scientific Meeting of the British Obesity and Metabolic Surgery Society in Leamington Spa, UK, from 22–24 January.
“Although bariatric surgery is the only evidence-based method of long-term weight control in obese individuals, the reduction in individual cardiovascular risk following bariatric surgery has not yet been quantified,” said presenter Dr Rami Radwan from the Institute of Metabolic and Obesity Surgery, Swansea, UK. “QRISK2 is a UK designed, validated and widely used algorithm to predict cardiovascular risk over a ten year period. In this study we calculated the QRISK 2 scores for patients’ pre- and post-bariatric surgery at our institute in an effort to objectively assess cardiovascular risk reduction following bariatric surgery.”
Rami Radwan
They reviewed all patients who had undergone bariatric surgery over a ten year period (June 2003 – June 2013) at their institute using the Welsh Institute of Metabolic & Obesity Surgery (WIMOS) database. All demographic and cardiovascular risk data was obtained and QRISK2 score was calculated pre- and post-operatively for all patients. Post-operative score was calculated at the point of longest available follow up duration.
A total of 250 patients were included in our cohort; 184 female, median age 36 years (range 24-59 years). Median follow-up post-operatively for all patients was 24 months (mean 34 months, range 1-109 months).
The majority of patients (n=100; 70 female) underwent a sleeve gastrectomy, 67 (26.8%; 45 female) patients had biliary-pancreatic diversion (BPD), 50 (20%; 39 female) patients had a roux-en-y gastric bypass (RYG), and 33 (13.2%; 30 female) were fitted with gastric bands.
Overall median pre-operative ten-year QRISK2 score was 5.6% (mean 9.4%, range 0.3%-45%) and the median postoperative ten-year QRISK2 score in these patients was lower at 4.4% (mean 7.2%, range 0.2%-36.1%); p<0.001.
“This study is the first to use a validated scoring system to assess ten year cardiovascular risk reduction in bariatric patients,” he concluded. “We have demonstrated a significant reduction in cardiovascular risk following bariatric surgery.
Co-authors of the study were Hazem Al-Momani, Scott Caplin and Jonathan Barry Welsh
A second study from researchers at North Tyneside General Hospital and James Cook University Hospital, Tyne and Wear, UK, assessed whether cardiovascular risk improved in bariatric patients following gastric bypass and if this improvement was sustained.
They analysed cardiovascular risk in 100 bariatric patients undergoing gastric bypass using a validated scoring system (QRISK II) to study their ten-year cardiovascular risk. Only patients who had at least two years follow-up were included. Paired t-test was used to assess if there was statistically significant difference in the QRISK. A total of 100 patients (M:F=1:6) with a mean age of 45.6 years (24-64 years), were included in they study.
The researchers reported that there was a statistically significant fall in the QRISK II score from baseline (6.328±6.75) at one year (3.62±3.45, p<0.0005), which persisted at two years as well (3.79 ± 3.58) (p<0.002).
This was more pronounced in patients with resolution/ remission of comorbidities like diabetes and hypertension. Patients who had long standing diabetes and whose diabetes persisted despite gastric bypass had less significant improvement in QRISK II score. Weight loss was significantly related to reduction in QRISK II.
“Patients undergoing gastric bypass have significant sustained reduction in their ten-year cardiovascular risk,” they concluded. “This is most pronounced in patients who had resolution of metabolic syndrome. We propose early referral to bariatric surgery to improve long-term cardiovascular morbidity.”
Read more

Obesity crisis: England’s fattest postcodes revealed
Shocking new data has revealed the true scale of England’s obesity crisis, with more than three-quarters of people in some towns and cities either overweight or obese.
Cumbria has been named the fattest county in England with 68.3 per cent of people overweight or obese, followed by Lincolnshire on 68.2 per cent and North Yorkshire and Staffordshire, both on 67.9 per cent.
Overall, 63.8 per cent of adults in England are overweight or obese, with a body mass index (BMI) of 25 or over.
Professor Kevin Fenton, director of health and wellbeing at Public Health England, said the new data will help all local areas ‘monitor their progress’ in tackling obesity.
‘There is no silver bullet to reducing obesity; it is a complex issue that requires action at individual, family, local and national levels,’ he said.
‘We can all play our part in this by eating a healthy, balanced diet and being more active.’
Find out the fattest locations in England below
UK obesity crisis: Cumbria named the fattest county in England
63.8 per cent of adults in England are overweight or obese, according to new data (Picture: PA)
Local authorities
- Copeland in west Cumbria (75.9% are overweight or obese)
- Doncaster in South Yorkshire (74.4%)
- East Lindsey in Lincolnshire (73.8%)
- Ryedale in North Yorkshire (73.7%)
- Sedgemoor in Somerset (73.4%)
- Gosport in Hampshire (72.9%)
- Castle Point in south Essex (72.8%)
- Bolsover in Derbyshire (72.5%)
- County Durham (72.5%)
- Milton Keynes (72.5%)
Counties
- Cumbria (68.3%)
- Lincolnshire (68.2%)
- North Yorkshire (67.9%)
- Staffordshire (67.9%)
- Northamptonshire (67.5%)
- Essex (67.3%)
- Derbyshire (66.9%)
- Nottinghamshire (66.4%)
- Norfolk (65.7%)
- Worcestershire (65.5%)
Regions
- North-east (68%)
- North-west (66%)
- West Midlands (65.7%)
- East Midlands (65.6%)
- Yorkshire and the Humber (65.4%)
- East of England (65.1%)
- South-east (63.1%)
- South-west (62.7%)
- London (57.3%)
Read more

Breast augmentation most popular procedure in the UK
There has been a dramatic increase in the popularity of plastic surgery in the UK, according to figures from the British Association of Aesthetic Plastic Surgeons (Baaps).
The number of nose jobs, face lifts and breast implant operations all soared by more than 10% last year. The biggest boom was in the popularity of liposuction - up by 41%. Baaps said it was "the most impressive rise in demand" since the start of the recession in 2008.
There were 50,122 cosmetic procedures in 2013 - a rise of 17% on the previous year. Baaps said the increase had been "across the board".
The top 10 procedures were:
- Breast augmentation up 13% to 11,135
- Eyelid surgery up 14% to 7,808
- Face and neck lifts up 13% to 6,380
- Breast reduction up 12.5% to 5,476
- Nose jobs up 17% to 4,878
- Liposuction up 41% to 4,326
- Tummy tucks up 16% to 3,466
- Fat transfer operations up 14.5% to 3,302
- Brow lifts up 17% to 2,138
- Ear corrections up 14% to 1,213
Breast enhancements were the most popular operation in women, while nose jobs were the cosmetic surgery of choice in men.
Rajiv Grover, a consultant plastic surgeon and president of Baaps, said: "Both the UK economy and the British public seem to be well on the way to regaining their shape with the most impressive rise in demand for cosmetic surgery we have seen since the onset of the recession in 2008.
AdvertisementBritish Association of Aesthetic Plastic Surgeons President Rajiv Grover said there were "risks as well as benefits" to cosmetic surgery
"The continued double-digit rise of cosmetic surgery underlines the fact that whether it is breast augmentation or anti-ageing procedures like face-lifting, the public are choosing tried-and-tested surgical methods rather than the magical-sounding quick fixes that fail to deliver promised results."
Tricky time
The reputation of the cosmetic surgery industry was brought into question during a scandal involving faulty breast implants.
A lack of record-keeping meant some surgeries were unable to tell their patients if they were affected by the recent scare over sub-standard PIP implants.
Health ministers described it as a "cowboy industry" steeped in "murky practices".
In January a new register was set up to record the details of every breast implant operation in England.
Fresh efforts are also being made to regulate adverts for surgery, to end the era of "win a boob job" competitions.
The industry was worth £750m in the UK in 2005, £2.3bn in 2010 and is forecast to reach £3.6bn by 2015.
Read more

Lap banding a long-term obesity solution: study
Lap band surgery is an effective long-term measure for managing obesity, according to a 15-year study of thousands of patients who have undergone the procedure.
The study, from Monash University’s Centre for Obesity Research and Education, analysed the results in 3,227 patients who had gastric banding between 1994, when the procedure was first introduced, and 2011.
It found on average patients undergoing the procedure had lost 26kg, or almost half of their excess weight.
The study, published in Annals of Surgery, also included a meta-analysis of all gastric banding studies that included weight loss data at or beyond 10 years.
“It shows, on average, the band patients going out beyond 10 years have lost 54% of their excess weight,” said Dr Paul O’Brien, director of the Centre for Obesity Research & Education & Emeritus Professor of Surgery at Monash University.
AAP
About one in four adults in Australia are obese, with the prevalence of the disease increasing rapidly from 8% in 1980 to 23% in 2008.
The National Health and Medical Research Council recommends bariatric surgery should be considered only if nonoperative measures, such as diet and exercise, have failed. And in that case it’s only recommended for patients with a BMI greater than 40, or with a BMI greater than 35 and a number of serious illnesses.
Because obesity is a chronic disease, Dr O’Brien and colleagues write in their paper that any proposed obesity treatment should be expected to demonstrate long-term durability to be considered effective.
“These results show that when you have a significant problem with obesity, a long-term solution is available,” Professor O’Brien said.
He added that there were also important ramifications for the control of type 2 diabetes, which was strongly associated with being overweight. “In obese patients with type 2 diabetes, weight loss after gastric banding can lead to effective control of blood sugar levels without the need for medication in about three-quarters of cases,” Professor O’Brien said.
The patients included in the study had followed the rules of their treating team regarding eating, exercise and activity and committed to returning permanently to the aftercare program.
“It’s a very important part of getting a good result,” Dr O’Brien said, adding that about 81% of patients had continued to return for care. About one in 20 patients had the band removed during the study period.
A review of the effects of bariatric surgery conducted by the Garvan Institute of Medical Research last year found some types or the surgery may cause bone loss, particularly when carried out on young people who have not yet reached their peak bone mass.
“Even though we don’t yet understand all the mechanisms, we can see that the more radical the procedure, the greater the bone loss long-term,” said Malgorzata Brzozowska, an endocrinologist from the Garvan Institute.
Dr O'Brien said while bone health was an important issue to consider after gastric bypass surgery, it wasn’t a problem after lap banding.
“We haven’t found a problem and we’re not expecting a problem with any deficiency because they should absorb food normally,” Dr O'Brien said.
Read more

Study finds LAGB can be used to prevent diabetes
Weight loss could be crucial in preventing patients with impaired fasting glucose (IGF) developing diabetes, according to a study published in Diabetologia. The authors from the Centre for Obesity Research and Education (CORE), Monash University,the Walter and Eliza Hall Institute, University of Melbourne, and the Baker IDI Heart and Diabetes Institute, Australia, report that patients who received a laparoscopic adjustable gastric band (LAGB) had a reduced risk of progressing from IFG to diabetes.
“We show that the rate of progression from IFG to diabetes is substantially reduced in obese people who undergo LAGB surgery…these findings strengthen the case for a randomised trial to determine whether LAGB surgery is a safe and cost-effective approach to preventing type 2 diabetes in this population.”
Study
The investigators note that patients with IFG are at high risk of developing type 2 diabetes and obesity is a major risk factor. Therefore, they assessed whether LAGB in obese patients with IFG reduced the risk of developing type 2 diabetes.
This retrospective cohort study looked at the outcomes of obese people with IFG who underwent LAGB and compared them with those of Australian adults with IFG from a population-based study (AusDiab).
A total of 3,174 patients underwent LAGB between October 1995 and August 2007, 333 (248 women and 85 men) had IFG (5.6–6.9mmol/l) and no history of diabetes or of glucose-lowering drug use. Of the 333 patients, 281 (84%; 210 women and 71 men) had follow-up weight and FPG data.
At five years, the LAGB patients lost an average of 25kg. After a minimum follow-up period of four years, 14 patients developed diabetes (12 women) and 169 did not. There was a strong relationship between the weight change and the occurrence of diabetes.
When they compared these results with those of 1,043 AusDiab patients who had IFG and were followed for five years, 65 AusDiab participants developed diabetes. Importantly, when they examined obese AusDiab patients, the incidence of diabetes increased significantly (p<0.001) and was greater than the LAGB group (p<0.02).
To assess whether banding was independently associated with diabetes, they combined the data from both groups, replacing percentage weight change with the presence or absence of LAGB surgery. They found that from 1,324 patients, LAGB was associated with a reduced risk of diabetes of more than 75% (OR 0.239 [95% CI 0.095, 0.571], p =0.004), with female sex and baseline FPG also significantly associated with progression to diabetes.
Conclusion
“Taken together with the findings of the multivariable analysis, we conclude that weight loss in obesity complicated by IFG prevents progression to diabetes,” the authors write. “This accords with the recent Swedish Obese Subjects findings, trials of weight loss drugs and other reports of remission of diabetes after medical or surgically induced weight loss.”
Read more

More than 2m need weight loss op resaerches say in the Belfast Telegraph
Operations for weight loss - also called bariatric surgery - such as the fitting of a gastric band or gastric bypass surgery, is currently available on the NHS to treat those with potentially life-threatening obesity.
Some 8,000 people receive the treatment each year, but researchers from Imperial College London say more than 5% of adults would qualify, more than 2.1 million people.
Their study, published in the Journal of the Royal Society of Medicine, found that despite evidence of the cost-effectiveness of weight loss surgery, surgery rates were estimated to be a third of the NHS's benchmark rate.
The number of people eligible for surgery "far exceeds" the estimated number of people having procedures.
Researchers, who examined the health of nearly 9,500 people, acknowledged the huge financial implications for the NHS if treatments were carried out in such greater numbers.
But they said more investment may be necessary to meet a growing need for the procedures.
According to NHS guidelines, weight loss surgery may be offered to those whose morbid obesity could kill them, or to people who are morbidly obese and who have a serious condition such as type 2 diabetes or high blood pressure that could be improved if they lost weight.
The study found that those meeting the criteria for bariatric surgery were more likely to be women, retired with lower educational qualifications and of lower socio-economic status.
It said: "Recent hospital episode statistic data show surgery rates from 2003/4 to 2009/10 have risen year on year in England; with rates highest in women and those aged 40-54 years.
"However, service delivery rates still fall significantly below the level needed to support all those who could potentially benefit."
Several factors contributed to surgery rates being so low, the study found.
Those with greatest need for surgery were more often in the lowest socio-economic groups, who are least likely to use healthcare services.
Read more

Study: BIORING is comparable to LAPBAND device
The adjustable BIORING gastric ring (Cousin Biotech) is as safe and effective as the LAPBAND ring (Allergan), according to the results from a randomised study1 presented at the French society of obesity surgery (SOFFCO), in June 2013, realized by Pr Chevallier.
The RESULTS confirm the outcomes from a previous abstract, ‘Randomized Controlled Study Comparing LAGB with Bioring and Lapband: One Year Outcome (Obesity Surgery 2009 19:953–1076, O-031, p 961)’, and adds to the growing body of evidence supporting the use of the BIORING gastric ring for treating morbid obesity.
BIORING gastric ring
The BIORING adjustable gastric band system is indicated for excess weight loss in people suffering from morbid obesity with a BMI>40 or 35 to 40 associated with at least one co-morbidity.
The adjustable gastric band is made of a supple silicone monoblock body with a unique bellow system, a silicone catheter labelled with arrows, a connector and a low profile injection port.
BIORING was designed to prevent complications and its unique bellow inflation system incorporates an extra low pressure system making inflation less traumatic. This bellow msystem is also designed to have a shock absorbing effectm to follow the natural peristaltic movements of the stomach. Its monoblock, pre-shaped band body helps avoid leakages and the supple silicone allows for a non-traumatic usage.
BIORING has a large surface of contact on the stomach to avoid slippage. It also facilitates a multidirectional distribution of forces. Following inflation of the device, mmultiple forces are spread in several directions, thus decreasing pressure on the stomach.
The BIORING adjustable gastric band system
The device’s unique self-adhesive port eases the implantation, with reduced operative time and less postoperative pain for the patient (no stiches are required). In addition, the larger surface of the septum facilitates saline injection to adjust the band and it improves patient comfort. According to the company, the BIORING can easily be inserted through a 12mm trocar and was specifically designed to avoid complications such as erosion, slippage and pouch dilation.
The BIORING, which was designed for the Pars Flaccida technique, offers a trauma free passage in the narrow retro-gastric tunnel with its streamlined components. In addition, its circular memory form allows encircling without pressure on the stomach.
Study
The randomised study1 was designed to compare the effectiveness and safety of two models of adjustable ring: The low pressure BIORING band and the high-pressure LAPBAND gastric ring.
The prospective and multicentre, randomised study reported the percentage of excess weight loss after 12 months, as well as the mortality and severe peri- and post-operative device-related complications.
Outcomes
The study included 59 patients: 28 patients received the BIORING gastric ring and 30 patients received the LAPBAND device. The study researchers reported no significant differences between the two groups regarding age, weight, frequency of complications and arterial pressure.
The outcomes reveal that there were no deaths and the rate of complications was comparable in both groups: six in the BIORING group and seven in the LAPBAND group (p=0.19).
At 12 months, the percentage of excess weight loss was 42.3±20.6% in the BIORING group and 36.5±19.9% in the LAPBAND group (p=0.269). In addition, the quality of life measured by the SF-36 score and the Impact of Weight on Quality of Life (IWQOL) was comparable in both groups at 12 months.
The study researchers were from CHRU of Lille, the European Hospital Georges-Pompidou. Paris, Bruxelles, Belgium and the Hôpital Louis-Mourier, Paris, France. They concluded “at 12 months the effectiveness and safety of the BIORING and ALLERGAN’s rings are comparable”.
References
1.Devienne M, Caiazzo R, Chevallier J-M, Himpens J, Verhelst H, Pattou F, Msika S, ‘Comparison of the laparoscopic implantation of an adjustable BIORING gastric ring versus the VANGUARD: Randomized prospective study’, Obésité Volume 8, Issue 2, June 2013, p 63-68, article 1.11
Read more

UK failing to address obesity problem
The National Obesity Forum in the UK has warned that the UK authorities are failing to address the scale the of the obesity problem and are underestimating the true scale of the obese catastrophe facing the nation.
“We are now seven years on from the Foresight Report,” said Professor David Haslam, the Forum’s chairman. “Not only is the obesity situation in Britain not improving but the Doomsday scenario set out in that report might underestimate the true scale of the problem. There needs to be concerted action.”
The 2007 Foresight Report concluded that half the population will be obese by 2050, however the National Obesity Forum claim that this scenario does not cover the true extent of the problem.
It says that the 2007 Foresight Report, which also predicted that obesity levels would cost the country nearly £50billion a year by 2050, may have underrated the scale of the emergency.
The Forum calls on health officials to introduce hard-hitting awareness campaigns, similar to those for smoking, to stem the problem and wants family doctors to discuss weight management with their patients.
“There is a lot more we can be doing by way of earlier intervention and to encourage members of the public to take sensible steps to help themselves but this goes hand in hand with government leadership and ensuring responsible food and drink manufacturing and retailing,” he added. “We need more proactive engagement by healthcare professionals on weight management, more support and better signposting to services for people who are already obese and more importance placed on what we drink and how it affects our health. We have seen hard-hitting campaigns against smoking and it is time to back up the work that is being done with a similar approach for obesity.”
Professor Kevin Fenton, director of health and well-being at Public Health England, said: “Obesity is an international problem. It is a complex issue that requires action at national, local, family and individual level. Everyone has a role to play in improving the health and well-being of the public, and children in particular.”
Read more

Ireland: 80,000 require bariatric surgery
An estimated 80,000 people are morbidly obese and require bariatric surgery in Ireland, the Irish Independent has reported.
According to the report, some 2% of the Irish population have a BMI>40. Dr Francis Finucane (Galway University Hospital), a consultant endocrinologist who specialises in obesity, has called for an increase in the number of bariatric procedures, a move which he believe would cut costs significantly.
"The prevalence of obesity in Ireland is pretty much the same as in England and the costs associated with it would be similar. We can't afford not to provide this intervention," he said.
Belgium Surgery Services is working togheter with Laya healthcare insurance for obesity/ bariatric surgery abroad.
For al patients that require more infromation don't hesitate to contact us or book a free of charge consultation at our clinic in Dublin, Belfast or Cork.
Read more

Best prices for gastric band, gastric sleeve and gastric bypass in Dublin, London, Belfast, Cardiff, Birmingham, Glasgow and Manchester
Belgium Surgery Services guarantees the best prices for obesity surgery in Belgium with our bariatric surgeon Dr Chris Debruyne at our hopistal in Brussels. (www.azjanportaels.be)
- gastric band: 4250€
- gastric sleeve: 6250€
- gastric mini-bypass: 7450€
- gastric bypass: 7750€
Read more

Free aftercare for gastric bypass and gastric sleeve surgery in Dublin, Manchester, London, Glasgow, Belfast, Birmingham and Cardiff.
Have your gastric sleeve or gastric bypass done by Belgium Surgery Services and receive Free aftercare at our clinics in Dublin, Belfast, Glasgow, Manchester, Birmingham, London and Cardiff.
- Personal coaching and e-mail support.
- Body composition baseline measurements taken.
- Long term goals for weight management discussed.
- Follow up consultation post operative to advise on food intake managment.
- Diet sheets, eating plan and monitoring log provided.
- Updated report to Dr Debruyne and his medical team.
Read more

15-year Lap Band results Ireland and UK
The largest published long-term study of laparoscopic adjustable gastric banding (LAGB) has reported that the procedure is a safe and effective solution for obesity, with 47% excess weight loss (EWL) after 15 years.
The results of the 15-year study, which were published in the journal Annals of Surgery, also includes a systematic literature review for weight loss at ten years or more supporting the view that LAGB is safer than Roux-en-Y gastric bypass. The review finds that the long-term weight loss outcomes and needs for revisional surgery of these two procedures are “not different”.
"These results show that when you have a significant problem with obesity, a long-term solution is available," said Professor Paul O'Brien, Centre for Obesity Research and Education, Monash University, Melbourne, Australia. "This surgery is safe and effective, and it has lasting benefits. Substantial weight loss can change the lives of people who are obese - they can be healthier and live longer."
Read more

Mini-gastric (one-anastomosis) bypass becoming a mainstream bariatric operation in Ireland and UK
Dr Chris Debruyne already preformed a few thousand mini -gastric bypass surgeries what makes him one of the most experienced surgeons in Europe in this field.
The MGB Consensus attendees all reported prior experience with other bariatric operations – Roux-en-Y gastric bypass (RYGB), gastric banding (GB) and sleeve gastrectomy (SG).
Technique
The laparoscopic operation (Figure 1) creates two components: first, a restrictive lesser-curvature gastric pouch; second, a 200 cm or longer jejunal bypass with a single antecolic gastro-jejunostomy (GJ) anastomosis, which leads to significant fat malabsorption.
Read more

Gastricband aftercare 2014 Ireland and UK
New dates and adorable aftercare package available for 2014.
Emergency services for gastricband available in the UK and IRELAND
Ask a member of our team for more information and get a free fill.
IRL: 00353(0)87 694 45 65
UK: 0044(0)753 0599 756
Read more

Gastric band Dublin clinic now open from 8 AM
Dear all,
From January 2014 our Dublin clinic will be open from 8am so you can visit us before your working day.
Please check clinics to book an online appointment.
Marie Stopes international
11 Berkeley Street
Phibsborough, Dublin 7
Read more
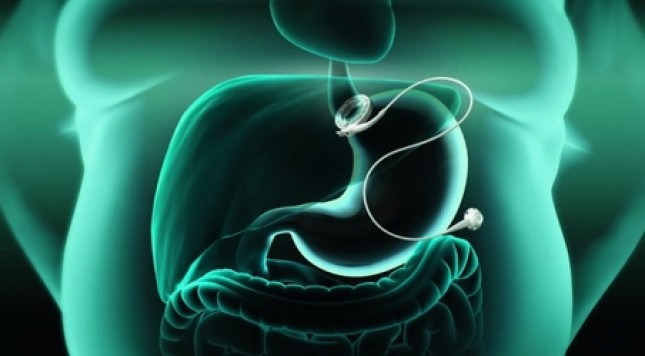
Bariatric surgery News Dublin, Manchester, Glasgow, London, Birmingham, Belfast, Cardiff, Cork, Edinburgh
Wendy Brown interview
The patient, not the procedure, is the key
Focus should be on patient care and follow up
Bariatric community can change the health and lives of many people around the world
Tuesday, February 19, 2013 - 12:12
Owen Haskins- Editor in chief, Bariatric News
The Centre for Obesity Research and Education (CORE), Monash University, Melbourne, Australia, recently published their 15-year Lap-Band outcomes which showed that the procedure is a safe and effective and resulting in 47% excess weight loss after 15 years. Bariatric News talked to Associate Professor Wendy Brown, director of CORE, about her experience with LAGB procedures, the importance of patient follow-up and why bariatric and metabolic surgeons need to concentrate on the benefits of all bariatric procedures.
According to Brown there are many important aspects to take into consideration when discussing bariatric surgery with patients, as part of their pre-operative assessment.
“I spend considerable time with patients before I operate and we talk about what their health problems are at the moment, their social situation, and what their expectations are from the band or any other bariatric procedure”, she says. “One important aspect of surgery is to manage people’s expectations; some patients expect to lose far more weight that is actually achievable, more than the 50-60 percent excess weight loss that we believe is possible.”
She stresses the importance of communicating to patients that the LAGB, or any other bariatric procedure for that matter, is not a ‘magic bullet’ solution:"It is simply not possible to perform any operation where by they can magically still eat and lose weight. What we emphasise to patients is that this is a life-changing procedure and we will be with them every step of the way,” said Brown. It is a life long journey.”
They also look at the patient’s home situation and whether they are in an environment where they are going to be supported. A support network – friends and family – is very important for patients.
She explained that at her institution, patients meet with the surgeon to discuss their options, prior to surgery. She also usually invites the patient to speak to a bariatric GP as patients often feel more comfortable about asking questions to a GP, rather than a surgeon. It also gives the patients the time and space to ensure they are ready for surgery, and they must be given every opportunity to ask the necessary questions.
Brown's centre does not offer patients a routine psychological evaluation, as she claims that there is little evidence this has any real value.
They have performed a study that found pre-operative psychological assessment did not add anything to the outcome of patients, it was an unnecessary cost and the psychologists did not find if particularly useful.
Although they have two psychologists at Brown’s clinic, they tend to see patients post-operatively to assess behavioural changes and assit with goal setting.
Interestingly, the team at Monash do not have regular multi-disciplinary team meetings. They have regular clinical meetings three to four times a year to discuss best clinical practice and difficult clinical issues, however, Brown explained that when they are discussing patients it tends to be very much on a one to one basis.
“My cancer multi-disciplinary team will discuss each and every patient," she said. "However, in our bariatric setting there is very little evidence that patient’s outcomes will improve if they are assessed and discussed by the whole team.”
A lot of patients would put weight on before surgery because they saw it as a last chance to eat the foods they enjoy. Prior to surgery, now Brown places her patients on a two week low-calorie diet. Although there is there no evidence that this results in better outcomes, she uses this as a marker to tell them two weeks before surgery that their journey starts now.
“I really wish we had a way of predicting how well a patient will do prior to surgery," she said. "We have looked at psychological indicators, physiological data, oesophageal manometry, metabolic make-up and syndrome, but we have not been able to identify any good preoperative predictors of who will do well and who will not."
Post-operative treatment
As their 15-year results demonstrated, LAGB is very effective. However, the team at Monash know that if a patient has not achieved about 25%EWL by three months, they are unlikely to achieve satisfactory weight loss.
“As a result, we are focusing more and more on intensive treatment in that early period, so if there are psychological issues or eating patterns or habits emerging, or other issues, we can address them early,” said Brown. “Usually, patients are still very motivated within the first three months and are very much part of the process so we try to attain as much weight loss as possible and hopefully this will carry on.”
“I sometimes think the information we provide before an operation is like reading a travel guide before you go to Paris. you read the information before you get there but it does not make much sense” said Brown. “Then you arrive in Paris and you read it again and it makes much more sense. So we try and put in a process so they can refer to the preoperative information after the operation, and have opportunity to revisit the information as they continue their journey.”
Patients do not routinely see the dietician pre-operatively: Brown feels as it offers no benefit to the overall outcome. The surgeon provides the patient with information about their diet, there is a concern that an additional meeting with the dietician would add to the "information overload" before the operation.
Patients see the dietician within the first few weeks of surgery so they can help them make the transition from semi-solid to solid food. Dieticians at their clinics run different programmes from one-on-one sessions to group sessions that offer advice on eating at restaurants, shopping and dealing with social situations, so it depends on the patient’s individual requirements and needs as to how often they require advice.
Similarly, the psychologist is very much on a needs basis, so if the patient is struggling with their eating or they have behavioural changes then they can arrange an appointment.
A patient’s first formal visit to the surgeon is about four weeks after their procedure, and this is when they usually have their first adjustment.
“We really make the focus of our visits about what they are eating and why, not about the band adjustment," says Brown.
They are encouraged to come back every three to four weeks for the first six months depending on their hunger, because controlling huger is seen as a key to success. After the first six months they are usually seen every three to four months, in some cases once or twice a year.
“There is a real emphasis on never losing touch," she says. "We want to make sure there are no complications and care for them as a metabolic surgeon should.”
She added that in Australia aftercare provision is paid for as part of thenational insurance coverage, allowing patients to receive excellent and extended follow-up.
The focus of patient treatment is on aftercare and Brown and her colleagues have adopted a holistic approach, which includes opening satellite clinics across Melbourne so patients can visit GPs or dieticians near their homes. The easier it is for patients to have access to advice on eating patterns, the more they feel involved.
Brown said that one positive aspect of the LAGB is that patients perceive the need to come in for a check-up as there is a prosthesis in place that needs occasional adjustment. Bypass or sleeve patients do not feel the necessity to visit their surgeon as they typically lose weight regardless of the visit.
Obesity is a chronic disease, and all procedures have better outcomes with a strong aftercare programme. The fact that the patient perceives a need for follow up with a band makes it easier to framework their care as a chronic disease.
Following patients in to the long term with intermittent phone calls is insufficient, she says, as they could have severe nutritional problems that the surgeon would be unaware of, and typically patients underestimate their weight.
“As with any chronic disease you need a chronic care plan. There has been an inappropriate perception in Australia that a patient who has a sleeve gastrectomy does not require follow-up, the so called “Sleeve and Leave” procedure. As metabolic surgeons we are changing a patient’s metabolism and we therefore have a professional responsibility to provide adequate after care for teh rest of that patient's life.”
With over 15 years experience with LAGB, the team at Monash University has written extensively on how the band work and movement of the bolus through the band. Now, they not only advise patients on what to eat but how to eat, emphasising to patients how important it is to eat slowly, chew your food.
“We are constantly re-enforcing the need to make the correct food choices and stressing the need to follow our 20/20/20 rule," says Brown. "Serve up your food on a small plate, use a small fork, chew the food 20 times, put the fork down for 20 seconds and it should take 20 minutes to eat that plate of food."
Bariatric community
Every treatment in medicine has an upside and a downside, and bariatric and metabolic surgery is no different. Obesity is a multi-factorial disease with biological, psychological and sociological contributors, and is very hard to control.
“Eventually, there will be some magic pill that fixes a patients metabolism," says Brown. “But until then, I think the message we need to tell patients, payers and referring doctors is that all bariatric surgery - whether it’s a band, bypass or sleeve - is safe, its effective and its far better than the any of the alternatives.
“The bariatric community has done itself a dis-service by focusing on which procedure instead of focusing on the benefits of all bariatric procedures. We have a great future as a profession, with enormous potential to change the health and lives of many people around the world, if we only we could stand together and stop fighting with each other.”
Read more